New work transforms our knowledge of how blood is formed
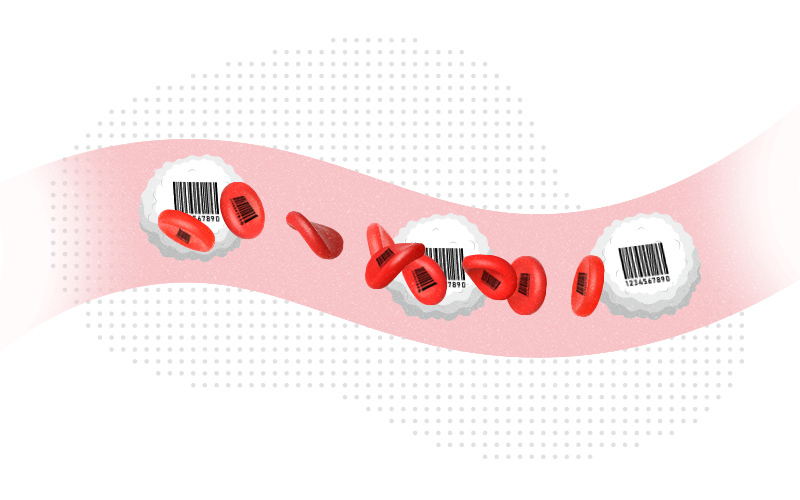
The origins of our blood may not be quite what we thought. In groundbreaking research, scientists in the Stem Cell Program at Boston Children’s Hospital used cellular “barcoding” techniques in mice to track the development of blood in real time — and found that blood cells originate not from one type of mother cell, but two.
“Historically, people have believed that most of our blood comes from a very small number of cells that eventually become blood stem cells, also known as hematopoietic stem cells,” says study leader Fernando Camargo, PhD, who is also affiliated with Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. “We were surprised to find another group of progenitor cells that do not come from stem cells. They make most of the blood in fetal life until young adulthood, and then gradually start decreasing.”
The researchers are now investigating whether humans also have these newly uncovered blood progenitor cells, known as embryonic multipotent progenitor cells (eMPPs). If so, further studies of these cells could potentially shed new light on blood cancers, especially those in children, and help make bone marrow transplants more effective. They could also inform new treatments for boosting aging people’s immune systems.
Cellular ‘barcodes’ reveal blood origins
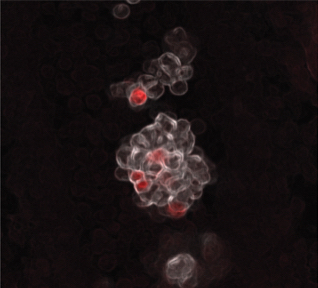
As described in the journal Nature, Camargo and his colleagues applied a barcoding technique they developed several years ago. It uses either CRISPR gene editing or an enzyme known as transposase to insert unique genetic sequences into embryonic mouse cells in such a way that all the cells descended from them also carry those sequences. Using these barcodes, the team then tracked the emergence of all the different types of blood cells and where they came from, all the way to adulthood.
“Previously, people didn’t have these tools, and the idea that stem cells give rise to all the blood cells was so embedded that no one attempted to question it,” explains Camargo. “By tracking what happened in mice over time, we were able to see new biology.”
Understanding the aging immune system
Through barcoding, the researchers found that eMPPs, as compared with blood stem cells, are a more abundant source of most lymphoid cells important to the immune responses, such as B cells and T cells. Camargo believes the decrease in eMPPs they saw over time may explain why people’s immunity weakens as they get older.
“We’re now trying to understand why these cells peter out in middle age,” he says. “This could potentially allow us to manipulate them with the goal of rejuvenating the immune system.”
In theory, there could be two ways to meet this goal: extending the life of eMPP cells, perhaps through growth factors or immune signaling molecules, or treating blood stem cells to make them more like eMPPs, through gene therapy or other approaches.
Unpacking blood cancers
Camargo is also excited about the potential eMPPs may hold for better understanding and treating blood cancers. For example, he thinks that myeloid leukemias, striking mostly older people, may originate from blood stem cells, while leukemias in children, which are mostly lymphoid leukemias, may originate from eMPPs.
“We are following up to try to understand the consequences of mutations that lead to leukemia by looking at their effects in both blood stem cells and eMPPs in mice,” he says. “We want to see if the leukemias that arise from these different cells of origin are different — lymphoid-like or myeloid-like.”
Improving bone marrow transplant?
Finally, the recognition that there are two types of mother cells in the blood could revolutionize bone marrow transplant.
“When we tried to do bone marrow transplants in mice, we found that the eMPPs didn’t engraft well; they only lasted a few weeks,” says Camargo. “If we could get eMPPs to engraft long term, they could potentially be a better source for a bone marrow transplant. eMPPs are more common in younger marrow donors than blood stem cells, and since they are primed to produce lymphoid cells, they could lead to better reconstitution of the immune system and fewer infection complications after the graft.”
Sachin H. Patel, MD, PhD, of the Stem Cell Program (now at University of California San Francisco) and Constantina Christodoulou, PhD (now at Bristol Myers Squibb) were co-first authors on the paper.
Learn more about stem cell research at Boston Children’s Hospital
Related Posts :
-

“A setback for a comeback”: Brody perseveres with Paget-Schroetter Syndrome
Baseball has been part of Brody Walsh’s story from the very start. Now 19 and a college sophomore, Brody pitches ...
-

Tough cookie: Steroid therapy helps Alessandra thrive with Diamond-Blackfan anemia
Two-year-old Alessandra is many things. She’s sweet, happy, curious, and, according to her parents, Ralph and Irma, a budding ...
-

A new druggable cancer target: RNA-binding proteins on the cell surface
In 2021, research led by Ryan Flynn, MD, PhD, and his mentor, Nobel laureate Carolyn Bertozzi, PhD, opened a new chapter ...
-

Unique data revealed just when Mickey’s heart doctors could operate
When Mikolaj “Mickey” Karski’s family traveled from Poland to Boston to get him heart care, they weren’t thinking ...