A toast to BRD4: How acidity changes the immune response
It started with wine. Or more precisely, a conversation about it.
“My colleagues and I were talking about how some people think drinking wine may be anti-inflammatory,” recalls Xu Zhou, PhD, from the Division of Gastroenterology, Hepatology, and Nutrition at Boston Children’s Hospital. “There’s no scientific ground for that, but we know wine is acidic.”
Around the same time, Zhou and his team were exploring a broader blind spot in immunology: the role of the tissue microenvironment (such as pH, oxygen, and salt concentration) in shaping immune function. While most research had focused on cellular messengers like cytokines, Zhou was curious about how the physical and chemical makeup of tissues might influence immune cells, especially in disease.
Inspired by their wine conversation and intrigued by these overlooked components, Zhou’s team launched a study to investigate how acidity affects immune cells. Their findings, published in Cell, show that a drop in pH can suppress immune responses by disrupting a protein called BRD4 — an important regulator of gene activity in immune cells. That small chemical shift could have big implications for treating inflammation-related diseases.
Acid, inflammation, and immune response
Inflammation is critical for fighting infection and injury, but too much can cause tissue damage. In serious conditions like sepsis, inflammation can lower blood pH, a state called acidosis. “Blood pH is normally quite stable in our body, ranging between 7.3 and 7.4. You rarely see anybody with a pH range beyond .1 unit from that very narrow, regulated range,” Zhou says. “In the case of patients with sepsis, having a pH around 7.2 is a really, really poor prognostic marker for survival.”
If acidity shows up consistently in severe inflammation, Zhou wondered: Could it be doing more than signaling disease? Could it be influencing how immune cells behave?
From wine to yeast: The missing piece
Zhou and his team tested this by exposing mouse and human immune cells to mildly acidic conditions (lowering extracellular pH from 7.4 to 6.5) and tracking changes in gene activity. They found that this small shift suppressed key immune transcriptional programs.
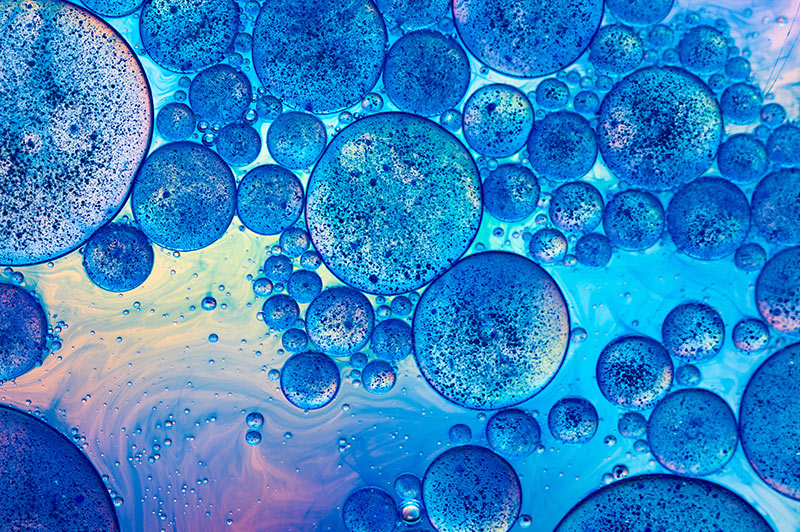
Using genetic tools, imaging, and chromatin immunoprecipitation sequencing (ChIP-seq), the team traced the immune-suppressing effect to BRD4 — a protein that helps switch on inflammatory genes. In acidic conditions, BRD4 lost its ability to form droplet-like clusters (called condensates) inside the nucleus, structures that are essential for its gene-activating role.
This mechanism had remained a mystery for years, until Zhou came across a study on pH sensing in budding yeast. The paper described a pH-sensitive protein that regulates gene expression with two histidine residues and a disordered protein loop — features it uses to sense acidity and adjust which genes are turned on or off. It proved to be the missing link: acidity disrupts BRD4’s condensates, reshaping gene expression in immune cells.
“You can imagine how surprising it was: people studying immune cells relying on something from yeast,” Zhou reflects. “But it worked.”
In both mouse and human cells, acidity disrupted BRD4’s ability to bind chromatin and activate genes, effectively blunting immune responses. That could explain why immune cells often struggle to perform in acidic environments like tumors or sites of chronic inflammation.
By uncovering how BRD4 responds to pH, Zhou’s team revealed a new molecular mechanism behind immune suppression that could be targeted in disease. The research points to pH as a lever that can dial immune activity up or down, depending on the need.
Laying the groundwork for future therapies
These discoveries point to new possibilities in immune therapy. “We can think about leveraging some findings we have into engineering CAR-T or cellular therapies, where we can make the immune cells resistant to these acidic microenvironments,” Zhou explains.
But the implications go beyond cancer: “We want to recover these lost functions in the immune systems,” Zhou says, “either limiting how strong they need to react, or bring the suppressed immune response back up.”
Zhou’s lab is now exploring strategies to stabilize BRD4 or regulate intracellular pH. “We can potentially build new models to look at pH inside tissues and small machines that can reverse most of these immune-suppressing activities,” he says. “This gives us the ability to understand how pH inside cells is disrupted during disease, and how we might control that intracellular environment to program immune response.”
While still in early stages, the discovery points to a new class of immune therapies that don’t just target immune cells, but also the environments they operate in. Future treatments might include drugs that protect pH-sensitive proteins like BRD4 or engineered immune cells that can function in acidic stress. That shift could open new therapeutic options for patients with cancer, autoimmune conditions, or chronic inflammation.
As Zhou puts it: “Just leveraging the knowledge across different spectra of science really helps us make new discoveries that haven’t been described before.”
Learn more about research in the Division of Gastroenterology, Hepatology, and Nutrition.
Related Posts :
-

Meet BORIS: A new culprit in drug-resistant cancer?
Like a Russian bot corrupting U.S. elections, or a new prime minister wreaking havoc in the U.K., a ...
-

AI-designed proteins open doors to new immunotherapies
Artificial intelligence (AI) is increasingly helping drive advances in science and medicine — including cellular signaling. In a recent study, published ...
-

A new druggable cancer target: RNA-binding proteins on the cell surface
In 2021, research led by Ryan Flynn, MD, PhD, and his mentor, Nobel laureate Carolyn Bertozzi, PhD, opened a new chapter ...
-

Exposing a tumor's antigens to enhance immunotherapy
Successful immunotherapy for cancer involves activating a person’s own T cells to attack the tumor. But some tumors have ...