Nerve block and a way out of pain after surgery

If she hadn’t dislocated her knee severely when she was 13, Paige Thornton probably wouldn’t have such strong feelings about pain. But most teenagers haven’t gone through an experience like hers: two surgeries at a hospital outside of Boston followed by weeks of agonizing pain and a year and half struggling to walk.
Blocks use local or regional anesthesia to reduce pain signals travelling along nerves to the brain. The technique can reduce pain and the need for narcotic medication both during and after surgery.
When she was 16, Paige and her parents agreed that a third surgery, this one at Boston Children’s Hospital, was her best chance of regaining mobility. But memories of the pain she’d endured, and the narcotic pain relievers she’d had to rely on for several weeks after her previous procedure, hung over their decision.
At Boston Children’s, an innovative pain management technique after surgery — called a nerve block catheter — changed her pain experience and aided her recovery.
Tumbling into a world of pain
Paige’s troubles began with a cartwheel. A dancer since she was 3, she’d done hundreds of them by the time she was 13. But in 2019, a cartwheel dislocated her kneecap so badly, she had to have surgery to repair the damage at a hospital near her home in southern Massachusetts.
Little over a year after her first surgery, Paige dislocated her kneecap again, this time in gym class. “It was a strange way to find out she’s extremely double jointed,” says Paige’s mother, Julie. This time, the same surgeon in southern Massachusetts performed a tibial tubercle osteotomy (TTO). The procedure involved cutting and repositioning her tubercle, a bump in the bone just below the kneecap. This, her family hoped, would make her knee more stable so Paige could get on with her life.

But two days after the operation, when the anesthesia wore off, Paige was in terrible pain. “We couldn’t get it under control,” says Julie, who remembers her daughter crying and writhing on her bed. “Her pain was a 10 out of 10 every day for more than a month. She missed SO much school that year due to continued pain.”
Once an active kid who’d spent hours goofing around outside with her friends, she’d looked forward to being active again. But even after the worst of the surgical pain subsided, she continued to struggle to walk. A nurse at her school suggested Boston Children’s.
A totally different experience
Paige and her parents met with Dr. Matthew Milewski in Boston Children’s Orthopedic Center a month and a half after her TTO surgery. “Right from the very beginning, it was a totally different experience,” says Julie. “Dr. Milewski spoke directly to Paige. The surgeon at the adult hospital talked to me and her dad, even though Paige was right there. She felt much more comfortable at Boston Children’s.”
Soon, Paige had a team of orthopedic and pain management specialists working together to help her walk without pain. Dr. Milewski met with her and her parents regularly — in person and via telehealth — to monitor the health of her knee.
Bearing weight on her leg, however, remained painful. A year and a half after her first TTO, Paige and her parents, in consultation with Dr. Milewski, opted for a second osteotomy. To manage her pain after surgery, Dr. Milewski suggested a nerve block catheter. After a conversation with the Home Analgesia Program, they decided to give it a try.
Over the hurdle of post-surgical pain
In June 2022, Dr. Milewski performed Paige’s second tibial tubercle osteotomy. Before she went home the next day, Dr. Walid Alrayashi, director of Regional Anesthesia, placed a thin tube under the skin near Paige’s knee. The tube was connected to an infusion pump that released a local anesthetic into the area at a slow and steady rate.
“It’s almost like your leg goes numb,” says Paige, describing the sensation of the nerve block. As expected, she experienced significantly less pain in the crucial days after her surgery. “Without the nerve block, the pain would be 100 percent, go down to 50 percent when I took a pill, and then go back to 100,” says Paige. “With the nerve block, the pain stayed at about 50 until it was gone.”

Five days after her third and final surgery, Paige removed the nerve block catheter at home while a clinician from the Home Analgesia Program team talked her through the process on a video call.
“The nerve block got us over the hurdle of those first few days,” says Julie. After that, all she needed was Tylenol.”
Finding her footing
The day after her surgery, Paige could walk with crutches and go up and down stairs. Six weeks after the operation, she ditched the crutches altogether.
“After the first TTO, I couldn’t walk without crutches for three months,” she says. “This time, I could bear all my weight on my leg without it killing me within a month and a half.”
These days, Paige is keeping busy with swimming, reading, and working two jobs. This fall, she got her driver’s license. “Just being able to return to normalcy in six months compared to the years of pain after the cartwheel — the difference is night and day,” says Julie.
Learn more about the Orthopedic Center and Home Analgesia Program.
Related Posts :
-

Interventional pain techniques bring Sadie relief
It’s hard for Sadie Doherty and her parents to remember a time when she hasn’t been in pain. ...
-

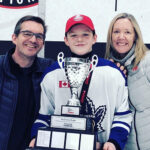
From Toronto to Boston: Osteochondritis dissecans, hockey, and hope
Hockey is a fast and physical sport. Players need to think and act quickly as their team members, opponents, and ...
-

For Kayla, post-surgical pain relief supports a lifetime of care
At 24, Kayla Regan is old enough to be the mother of some of her fellow patients at Boston Children’s ...
-

Always an athlete: Drew and Legg-Calve-Perthes disease
When he looks back on the diagnosis that forced him to stop playing sports entirely for more than a year, 11...