From bench to bedside: A promising option for unremitting ulcerative colitis
Many existing treatments for inflammatory bowel disease, like Remicade® and Humira®, work by blocking inflammatory cytokines such as tumor necrosis factor (TNF) and interleukins IL-12 and IL-23, which are over-produced in autoimmune disease. But few patients with ulcerative colitis get complete relief from these drugs.
A small but promising open-label clinical trial, published recently in Gastroenterology, suggests a new option: low-dose IL-2 (Proleukin®).
In high doses, IL-2 is pro-inflammatory and is used to fight cancer. But in low doses, it stimulates the T regulatory cells (Tregs) that suppress inflammation and are thought to be in short supply in ulcerative colitis.
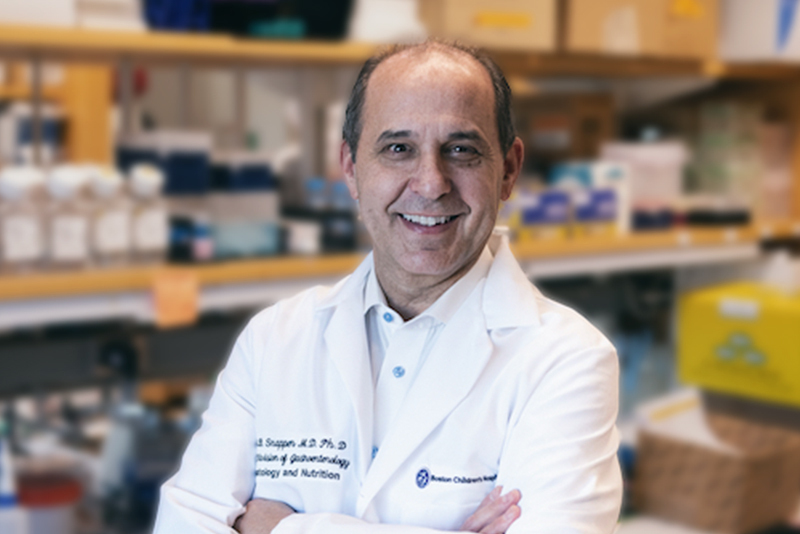
“The current therapeutic arsenal for ulcerative colitis is grossly inadequate; more than half of patients do not go into long-term sustained remission,” says Scott Snapper, MD, PhD, chief of the Division of Gastroenterology, Hepatology, and Nutrition at Boston Children’s Hospital and co-principal investigator on the study. “We and others have had the thought to try to enhance the natural population of T regulatory cells, instead of blocking pro-inflammatory processes.”
Stimulating T regulatory cells
The Phase 1b/2a trial followed promising studies of IL-2 in a mouse model of colitis in Snapper’s lab. Conducted in collaboration with co-principal investigator Jessica Allegretti, MD, MPH, at Brigham and Women’s Hospital, the trial enrolled 26 adults with moderate-to-severe ulcerative colitis in whom at least one prior therapy had failed. Patients received subcutaneous IL-2 in a dose-escalating design and were assessed at eight weeks with Mayo scores, which measure stool frequency, blood in stools, and mucosal appearance on flexible sigmoidoscopy.
After eight weeks of daily treatment, many patients showed dramatic symptom relief and often remission. Of the 19 who completed treatment, 10 (53 percent) had a clinical response, and four (21 percent) had a complete remission. Of the three IL-2 doses tested, the most effective was 1 x 106 IU/m2/day, producing a clinical response in nine of 13 patients (69 percent) and remission in four (31 percent).
Tregs increased in the blood of all clinical responders and 12 of 13 non-responders. The study was only able to assess Tregs in the intestine at 0 and 8 weeks, so it could have missed a change during active treatment. There were no serious adverse reactions; most side effects were injection site reactions, fever, and malaise.
Future directions
Snapper hopes these findings will encourage manufacturers to sponsor placebo-controlled Phase 2 and Phase 3 studies in larger populations, including children. New versions of IL-2 are becoming available that may be even more effective, he says.
“Because of the good safety data, I think there’s promise for trying this in children over 14,” he says. “This is an exciting future potential option for patients.”
Snapper and Allegretti are now testing low-dose IL-2 in patients with Crohn’s disease. The lab is also investigating genetic or other biomarkers that predict whether a patient will respond.
Learn more about research in the Snapper Lab or refer a patient to the Division of Gastroenterology, Hepatology, and Nutrition.
Related Posts :
-

Identifying specific markers in blood may improve diagnosis of IBD in children
New research may lead to improved methods to diagnose inflammatory bowel disease (IBD) in children. This could be ...
-

Yoga program helps children and teens better manage IBD and stress
In a dimly lit room, about a half dozen teens stand quietly, each trying to balance on one leg. The ...
-

Could fecal transplants heal Crohn’s and colitis in children? Two trials are set to find out
Could an exciting potential treatment for inflammatory bowel disease (IBD) be found in the gastrointestinal tract itself? That’s the ...
-

Shaping our intestinal microbiome: What makes certain microbes more ‘fit’?
We now know the microbes that live in our intestines — often called our microbiome — influence our health in many ways. ...