A global view of rheumatic disease during COVID-19

COVID-19 is bringing new challenges to many people with underlying rheumatic disease who already are immunocompromised by the very nature of their illnesses or the medications used to treat them. To help manage those uncertainties in the current climate, Boston Children’s Hospital is participating in two surveys: one collecting information from rheumatologists, the other directly from patients.
We want to understand the social, psychosocial, emotional, and physical impacts of the pandemic on these vulnerable patients, and hopefully offer advice and insights about how to manage their medicines and improve their overall well-being,”
– Jonathan Hausmann
Developed by the COVID-19 Global Rheumatology Alliance (GRA) in March 2020, the goal of the surveys is to better understand the impact the pandemic has had on rheumatology patients around the world —children and adults — regardless of their COVID-19 status.

“The big goal is to try to understand what is going on with patients with rheumatic disease during the pandemic and to provide some useful insights into what can and should be done for these patients,” says Jonathan Hausmann, MD, of the Rheumatology Program at Boston Children’s and member of the COVID-19 GRA Steering Committee. “We want to help patients best manage their rheumatic disease now and get the information out there as soon as possible.”
Provider-entered survey includes pediatric and adult patients
The Healthcare Provider Entered Registries houses information from several databases of adults and children with rheumatic disease with COVID-19. Boston Children’s manages data collection and analysis of the pediatric portion of the database known as the COVID-19 Global Pediatric Rheumatology Database.

“The goal is to find out which medications put patients at greater or lesser risk of having severe COVID-19-related problems,” says Marc Natter, MD, of the Computational Health Informatics Program (CHIP) at Boston Children’s and lead investigator of the pediatric database. “The intent is to follow these patients with rheumatic diseases over time to understand the effects the virus has on different rheumatic diseases.”
Currently, the provider-entered survey includes information from about 3,900 adult patients and 50 children with rheumatic disease and COVID-19 from nearly every continent.
“Because pediatric rheumatic diseases are very different than adult diseases, we have to understand how COVID-19 acts in these patients and how it is changed by different rheumatic diseases,” says Natter. “We also want to know if the virus ends up triggering pediatric rheumatic diseases which we often see with other viruses.”
The Patient Experience Survey
Described in a paper in Arthritis Care and Research, the patient-reported Patient Experience Survey recruits input from adults and parents of children with rheumatic diseases. To date, over 13,100 responses have poured in from children and adults in over 90 countries, including about 790 patients with COVID-19, almost all adults. Among the responses are nearly 500 related to children with rheumatic diseases.
“We want to understand the social, psychosocial, emotional, and physical impacts of the pandemic on these vulnerable patients, and hopefully offer advice and insights about how to manage their medicines and improve their overall well-being,” says Hausmann, who leads the Patient Experience Survey.
Immediate snapshot of the landscape
Because the survey collects data from people with rheumatic diseases, the information reflects real-time conditions.
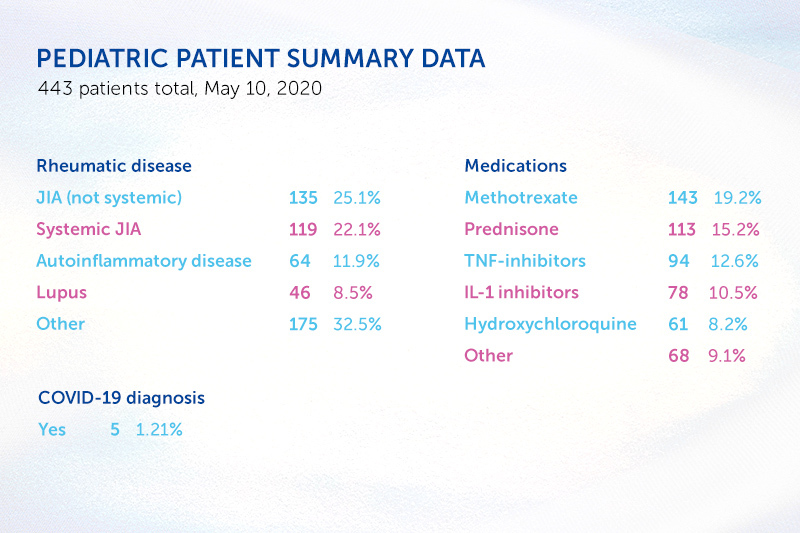
As an example, the team has learned that most of the 500 children with rheumatic disease in the patient registry take some type of immunosuppressive drug. Yet, only a handful reported infection with COVID-19, and none required hospitalization. “Our results suggest that, like otherwise healthy children, those with immunosuppression are at low risk of COVID-19 infection and low risk of severe outcomes should they become infected,” says Hausmann
First papers published
Now, some of the first results from the provider survey among adults are starting to come in. In a paper in the Annals of the Rheumatic Diseases, the team reported on the characteristics of 600 patients from 40 different countries with rheumatological disease and COVID-19. They found an association between taking ≥10 mg/day of a glucocorticoid like prednisone and a higher probability for hospitalization. Anti-tumor necrosis factor medication decreased the odds of hospitalization. Other common anti-rheumatic drugs like disease-modifying anti-rheumatic drugs, biologics, JAK inhibitors, and non-steroidal anti-inflammatory drugs did not show a link with higher hospitalization rates.
“Because both surveys have some of the same questions, we hope to soon compare information from the Patient Experience Survey with that from the physician-entered registry,” says Hausmann. “The more responses we have to the same questions the more power we will have to show effects and provide useful information quickly.”
Related Posts :
-

Promising advances in fetal therapy for vein of Galen malformation
In 2024, Megan Ingram* of California and her husband were preparing for the birth of their third child when a 34-week ...
-

The hidden burden of solitude: How social withdrawal influences the adolescent brain
Adolescence is a period of social reorientation: a shift from a world centered on parents and family to one shaped ...
-

A toast to BRD4: How acidity changes the immune response
It started with wine. Or more precisely, a conversation about it. "My colleagues and I were talking about how some ...
-

A unique marker for pericytes could help forge a new path for pulmonary hypertension care
Pulmonary arterial hypertension (PAH) is a rare condition that’s difficult to treat. The hallmarks of the disease — narrowing of ...





