Blood across our lifetimes: An age-specific ‘atlas’ tells a dynamic story
The stem cells that form our blood, also known as hematopoietic stem cells (HSCs), are with us throughout our lives. A new study reveals how HSCs ramp up and pivot their activities depending on the body’s needs at the time, from before we’re born until old age.
Researchers at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center, led by Grant Rowe, MD, PhD, and Hojun Li, MD, PhD, have produced an “atlas” of blood development that they believe is the most detailed and comprehensive to date. The work also shines a new light on leukemia and preleukemia.
As detailed in Nature Methods, Rowe, Li, and their colleagues started by gathering existing data characterizing HSCs at different stages of life. These data sets turned out to be hard to combine, since they were acquired in different ways using different measures, and did not capture key moments of change during the lifespan. To fill in the gaps, the team directly collected HSCs from 26 human donors. This enabled them to capture 22 time points from as early as 10 weeks after conception to age 77.
That wasn’t an easy task. Collecting the samples took about five years, starting when Rowe and Li were both clinical fellows. Samples came from surgical cases around the Boston area as well as bone marrow transplants, says Li, who is now at University of California San Diego.
“We went above and beyond so we could see the whole age spectrum in a consolidated way, without confounding factors,” says Rowe, who directs the Bone Marrow Failure Clinic at Dana-Farber/Boston Children’s. “This allowed us to feel really confident in our conclusions.”
The story of our blood
In all, the researchers genetically profiled more than 58,000 individual HSCs and blood progenitor cells using single-cell RNA sequencing. This revealed what genes HSCs turned on and off at different points in the lifespan. “Because we analyzed single cells, we could see the genetic programs controlling these changes in specific types of blood precursors,” Rowe says.
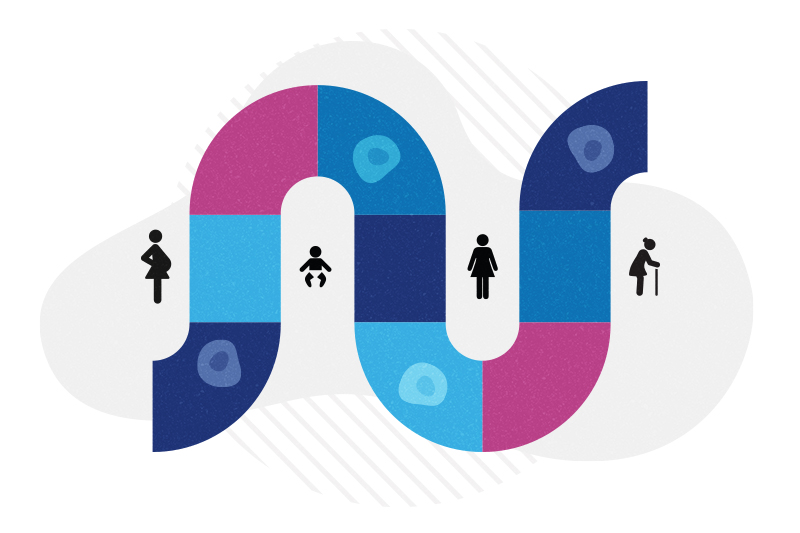
The story unfolds like this:
Before we’re born, HSCs rapidly multiply from just a handful of cells to robust populations in the liver (the main blood-forming organ during early gestation), ultimately taking up residence in our bone marrow.
HSCs then focus on making different types of blood cells. Early in gestation, the predominant cell type made is myeloid cells such as macrophages, which support organ development, and then red blood cells to meet a growing fetal demand for oxygen as the body grows.
As birth approaches, and through childhood, HSCs focus on producing virus-fighting lymphocytes. In adulthood, HSCs are in a relatively steady state, “kind of just maintaining things,” says Rowe.
But that changes as people start to age.
“Later in life, HSCs start to falter,” Rowe says. “They’re less effective at producing lymphocytes, and make myeloid cells by default. Sometimes they expand and create a premalignant state, which corresponds with the known higher risk of blood cancers in old age.”
Age-related programs in blood cancers
It’s known that cancerous cells can sometimes revert to an immature, stem-like state, making them more aggressive. The researchers wanted to compare genetic programs in these cells with age-specific genetic data from their HSC database. Looking at acute myeloid leukemia (AML) cells, they found that cancers tended to have a poor prognosis if their genetic programs resembled signatures of HSCs and progenitor cells in early life.
This was true regardless of the patient’s actual age, they found.
“Blood cancers are believed to be much worse if they activate fetal-like programs,” says Li. “We’re the first to truly demonstrate this by looking at the whole age continuum.”
This finding suggests that both children and adults with leukemia might benefit from reprogramming to help their cancer cells “grow up,” the researchers say.
A reference point for studying disease
The atlas will help support research on a variety of blood disorders and cancers, including childhood and adult leukemias and clonal hematopoiesis, a potential precursor to leukemia in which people, as they age, acquire mutations that enable certain blood cells to multiply faster than others.
“We believe that this resource will be important in understanding both childhood and adult blood diseases and how they differ,” says Rowe. “Childhood blood diseases are different from adult blood diseases. This will refine our understanding of why that is.”
To help move the field forward, Rowe, Li, and colleagues have created an open-access web resource to allow other researchers to browse their age-specific data and conduct their own research.
Explore research labs and clinical trials at Dana-Farber/Boston Children’s.
Related Posts :
-

Preventing leukemia by preventing rogue blood cells from taking over
As we age, many of us acquire mutations that cause some of our blood stem cells to multiply faster than ...
-

Could leukemia be stopped before it starts?
Acute myeloid leukemia (AML), a blood cancer affecting both adults and children, requires more than one genetic “hit” to develop. ...
-

Curbing blood cancers by teaching immune cells to kill mutant stem cells
Blood stem cells, which give rise to all of our blood cell types, undergo a quality assurance process after they’...
-

A universal gene therapy for Diamond-Blackfan anemia is poised for clinical testing
Diamond-Blackfan anemia (DBA), first described at Boston Children’s Hospital in 1938, is a rare blood disorder in which the bone ...