ctDNA: Bringing ‘liquid biopsies’ to pediatric solid tumors
Our blood carries tiny amounts of DNA from broken-up cells. If we have cancer, some of that DNA comes from tumor cells. Studies performed with adult cancers have shown that this circulating tumor DNA (ctDNA) may offer crucial clues about tumor genetic mutations and how tumors respond to treatment.
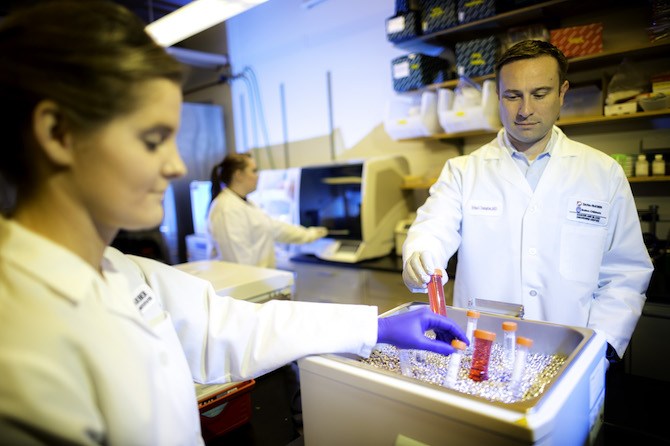
Brian Crompton, MD, with colleagues at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center and elsewhere, is now working to bring ctDNA “liquid biopsies” to pediatric solid tumors as well. The researchers hope that these blood tests will eventually improve early detection, choice of treatment and monitoring of young patients with these diseases without having to sample the tumor itself.
ctDNA: Gauging solid tumors with a blood test
In the last year, this team has shown that ctDNA can be detected and measured in patients with five of the most common pediatric solid tumors: Ewing sarcoma, osteosarcoma, neuroblastoma, alveolar rhabdomyosarcoma and Wilms tumor.

The scientists also found early correlations between ctDNA liquid biopsy findings and cancer progression in two pediatric bone cancers, Ewing sarcoma and osteosarcoma.
Liquid biopsies potentially could aid in tailoring treatments for both bone cancers — for example, by helping to predict which young patients will respond well to treatments, which can’t be done with current tools.
“If we could identify patients who have a very high risk of not being cured, we could potentially give them a more intense therapy or a different therapy, or enroll them in an experimental regimen,” Crompton says. “Detection and quantification of ctDNA could be one way to identify these high-risk patients.”
Rethinking ctDNA for kids
Applying ctDNA to pediatric solid tumors requires developing new approaches. “We can’t just take adult ctDNA assays and apply them to pediatrics, because the patterns of genetic mutations we see in children with cancer are completely different than the patterns of mutations we see in adults,” Crompton says.
We believe we will one day be able to use ctDNA to identify children who could be cured with reduced-intensity therapy, which could lessen long-term side effects.
In adult cancers, ctDNA analyses typically highlight point mutations — changes in a single “letter” of the genetic code. But pediatric cancers are different: ctDNA analyses generally must focus on structural changes in the DNA, such as translocations (rearrangements of DNA between chromosomes) or changes in the number of copies of a gene.
Adding to the challenge, researchers can’t always collect tumor biopsies from every child. “We want to be able to detect ctDNA with high confidence without ever having genetically profiled the tumor,” Crompton says.
Validating liquid biopsies
In a critical first step, described in PLOS One in December 2017, the researchers simplified the requirements for blood sampling, a particular concern among young cancer patients. They showed that a type of blood collection tube used to collect ctDNA also is suitable for gathering the patient’s own normal DNA. Simplifying the collection of blood samples “was really helpful in assuring that samples from liquid biopsy will be banked nationally for kids with any solid tumor,” says Crompton.
The multi-institutional team then went on to develop two methods for testing ctDNA. One assay was designed to capture DNA translocations in diseases such as Ewing sarcoma, primarily concentrating on regions of the genome where these translocations are likely to occur. The second, building on a tool created by the Broad Institute of MIT and Harvard, counts chromosomal copy number changes, which usually are present in high volume in osteosarcomas.
In the long run, we want to monitor how tumors evolve in response to therapy, by profiling the DNA every month for example. We can’t do that with a surgical biopsy.
Next, in an article published in July in JCO Precision Oncology, the scientists showed that ctDNA could be measured in the five types of solid pediatric tumors, in at least half of patients. The study also identified genomic markers of poor outcomes.
ctDNA in Ewing sarcoma and osteosarcoma
Finally, a paper in the British Journal of Cancer in August showed that detectable ctDNA identified with these assays was prognostic for outcomes in localized Ewing sarcoma and osteosarcoma.
Crompton is now working with Dana-Farber’s Steven DuBois, MD, MS, and David Stephen Shulman, MD, to launch a multi-institutional prospective study that will probe ctDNA in greater depth among patients with these two diseases.
The study’s primary goal is to confirm findings from its original patient samples, and to explore whether treatment-induced changes in ctDNA could be even more predictive of whether a patient’s disease is sensitive or resistant to therapy.
“In the long run, we want to monitor how the tumors evolve in response to therapy, by profiling the DNA every month for example,” says Crompton. “We can’t do that with a surgical biopsy, because we can’t operate on a patient every month. But we routinely draw blood samples every month for patients who are on therapy, so getting an extra tube of blood to do a liquid biopsy is simple.”
Lessening side effects, detecting recurrence
In the future, Crompton and his team hope to see an even broader impact.
“We believe that we will one day be able to use ctDNA to identify patients who could be cured with reduced-intensity therapy, which could lessen the risk of long-term side effects,” he says. “We also believe these assays could be used to monitor patients for early signs of relapse, when treatment may be more successful, and even for early detection of malignancies in families at high risk of developing cancer.”
Learn more about solid tumors in children.
Related Posts :
-

A true hero’s journey: How a team approach helped Wolfie overcome pancreatitis
Wolfgang, affectionately known as “Wolfie,” is a bright and energetic 7-year-old with a quick wit and a love for making ...
-

A case for Kennedy — and for rapid genomic testing in every NICU
Kennedy was born in August 2025 after what her parents, John and Diana, describe as an uneventful pregnancy. Soon after delivery, ...
-

The journey to a treatment for hereditary spastic paraplegia
In 2016, Darius Ebrahimi-Fakhari, MD, PhD, then a neurology fellow at Boston Children’s Hospital, met two little girls with spasticity ...
-

A toast to BRD4: How acidity changes the immune response
It started with wine. Or more precisely, a conversation about it. "My colleagues and I were talking about how some ...





