Diagnosed with clubfeet before he was born: Gabriel’s story

Cheryl Bratt and her wife, Sue, expected a routine visit when they went in for their 18-week ultrasound. Cheryl, a professor, had scheduled the test before her morning class. The radiologist was reassuring through the entire ultrasound — until the end. “Then she told us the baby had clubfeet and we needed to see a specialist.” Just like that, these expecting parents faced an unexpected diagnosis.
Clubfoot causes the front of the foot to turn inward and the heel to point down. As many as four children out of every 1,000 are born with clubfoot. Like about half of children with the condition, the ultrasound showed that Cheryl and Sue’s baby would have clubfeet on both sides.
Questions and fears about clubfoot diagnosis
The news came as a shock. Cheryl’s pregnancy with their first child, Ilan, had been easy and issue-free. “We were thrown. We didn’t know what the diagnosis meant.” The couple worried that clubfoot might be the first sign of a more serious birth defect.

Cheryl’s obstetrician referred the couple to the Maternal Fetal Care Center for further screening. Within days, they had their first meeting scheduled with Dr. Collin May of the Lower Extremity Program.
Understanding clubfoot treatment
Questions and answers about clubfoot
Why didn’t an earlier ultrasound detect Gabriel’s clubfeet?
Though clubfeet are probably present at an early stage of development, they can’t be distinguished from normal embryonic foot position until the later stages.
How definite is this diagnosis?
The accuracy of an ultrasound clubfoot diagnosis depends on the severity of the condition. Clubfoot that appears severe on an ultrasound has a 94 percent chance of being accurate. For moderate clubfoot, 70 percent of ultrasound diagnoses are accurate, and 25 percent of mild clubfoot diagnoses are accurate.
What is the risk that our child will have another condition in addition to clubfoot?
Clubfoot can be a feature of a more serious condition, however, such conditions are quite rare. The vast majority of children with clubfoot do not have other developmental issues.
The question of whether something she had done might have caused the deformity had worried Cheryl since she first got the diagnosis. “Right off the bat, Dr. May told us this was not my fault,” she says. “He understood that we were anxious and afraid.” They also wanted to know why an earlier ultrasound hadn’t detected the condition and whether the diagnosis meant their child was at greater risk for other birth defects.
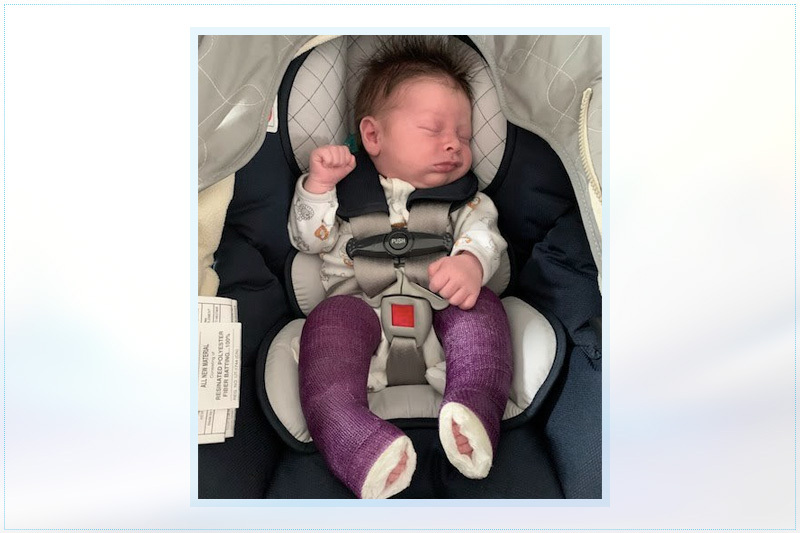
Treating clubfoot is not invasive but takes time and commitment. Within a few weeks of birth, the child’s feet are repositioned and placed in leg casts to hold them in position for a week. After several cycles of casting and minor surgery, children graduate to a brace. Nightly bracing continues for the next four to five years.
By the end of their meeting, Cheryl and Sue understood how their baby’s feet would be corrected. They knew the treatment would be challenging and take years, but felt reassured to have met the clinicians who would be involved.
“Dr. May and his team put us very much at ease. It was obvious they had worked with hundreds of families in our position and knew what they were doing.” Gabriel was due in four months. Dr. May asked Cheryl and Sue to let him know when he was born so he could stop by and say hello.
Gabriel’s clubfoot journey begins
Cheryl gave birth to Gabriel on February 2. Since the 18-week ultrasound, she’d wondered if his clubfeet would make it difficult for her to bond with him. “But when I saw his feet, they were adorable. I just loved them. I’m glad they’re corrected but it didn’t impact our bonding.”
As promised, Dr. May stopped by to meet the new baby. Three weeks later, on February 25, Gabriel’s clubfoot correction began.
Treating Gabriel’s clubfeet
Timing was on Gabriel’s side. He was several weeks into his clubfoot correction by the time Boston Children’s cancelled non-urgent procedures to prevent the spread of COVID-19. Because his treatment was already underway, Gabriel’s clubfoot correction continued on schedule.

Adjusting to the clubfoot brace
Now 6 months old, Gabriel only has to wear his brace at night. However, he and his moms have faced some challenges along the way. One cast had to be changed after Gabriel cried for a solid day and a half after a correction. A few times, his brace has caused heat rash and pressure sores. “We found everyone at Boston Children’s to be incredibly responsive,” says Cheryl. “They provided immediate support when we needed them.”

Gabriel may be delayed in crawling and walking, but has already figured out how to roll over wearing his brace. To Cheryl’s relief, the treatment has not seemed to cause him significant pain or upset, which she feared it might. “This is normal for him,” she says. “He hasn’t known anything different.”
Looking back on early fears about clubfoot treatment
If Cheryl could go back in time, she would reassure herself and Sue about Gabriel’s clubfeet. “It’s just one of the many things he’ll experience as a child” she says, “It’s part of who he is as a baby, but we don’t expect it to cause any long-term complications or difficulties. Although clubfoot requires a commitment to the years-long treatment plan, it is much more manageable than we thought it would be.”

Learn more about the Lower Extremity Program.
Related Posts :
-

When your baby has clubfoot: Answers for expecting parents
Treatment for clubfoot usually begins within a few weeks of a child’s birth. With prenatal ultrasound, parents often learn ...
-

How a meniscal transplant made me a Boston sports fan
I was in kindergarten when my knee started popping and cracking. My parents and I didn’t know it at ...
-

Hard and beautiful at the same time: Five lessons of raising a medically complex child
When they learned they were expecting a baby, Michelle and Stephen Strickland were delighted. The South Carolina couple looked forward ...
-

3D imaging could become standard practice in orthopedics. Here’s how.
It took a trained eye to see the abnormality on the patient’s X-ray. There, hidden behind the acetabulum was ...





