Utilizing engineering tools from the aerospace industry to repair hearts
When an 18-year-old patient from North Carolina recently presented at Boston Children’s Heart Center with an enlarged right atrium that made the flow through his Fontan circulation very inefficient, David Hoganson, MD, decided to utilize a new set of tools borrowed from the aerospace industry.
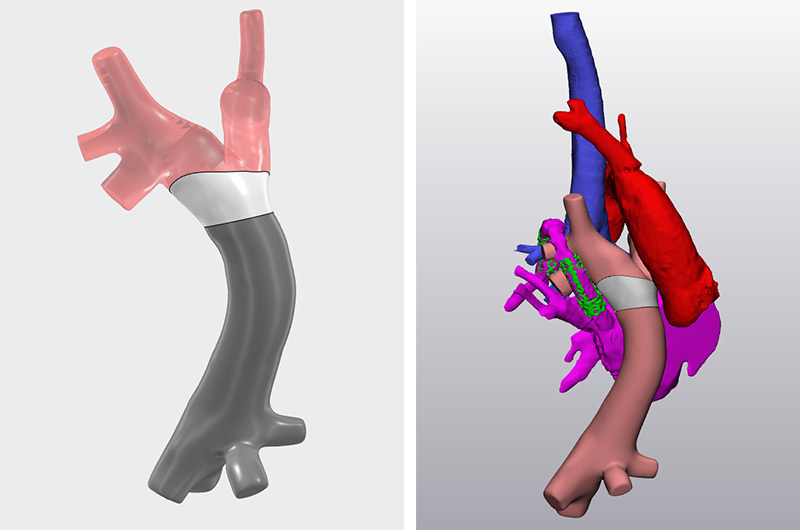
“We have been collaborating with Dassault Systemes for over a year now, using some of their simulation and engineering tools to better plan complex operations,” says Hoganson. “When this patient came up, we were already well down the path of developing a process to make aortic arch patches prospectively designed to fit kids perfectly. So when we determined he needed a cuff, which has complex curvature similar to the aorta patches, we realized we had the tools and expertise to create it.”
Using computer simulations and flow modeling
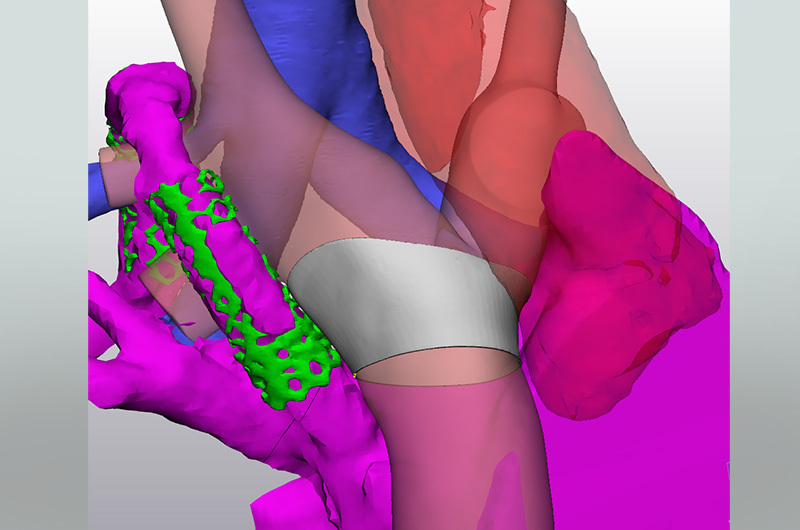
Before creating the cuff, Hoganson and his team ran a series of computer simulations of the surgery procedure using Dassault’s software and also modeled flow through the planned surgical reconstruction, which is now part of their standard procedure when planning for complex heart surgery. Computer flow modeling through the patient’s Fontan circulation showed the energy loss with the swirling flow, and predicted a 15 percent reduction in energy loss by placing a transition cuff placed between the conduit and pulmonary artery branches, converting the swirling flow in the dilated right atrium to smooth laminar flow in extracardiac Fontan.
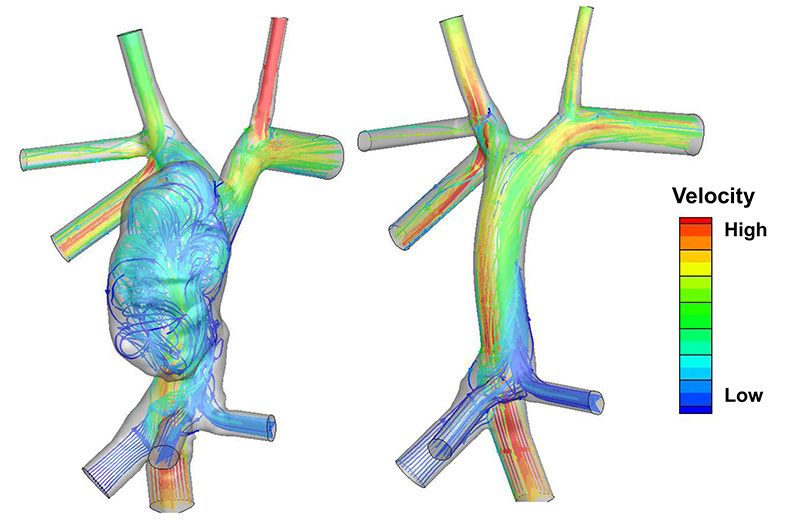
“Given the large size of the entrance into pulmonary arteries (38mm diameter) compared to the size of the conduit (20mm diameter), a special cuff had to be designed to create a smooth transition between the conduit and the native pulmonary arteries,” says Hoganson. “Utilizing 3-D modeling and flow simulation, we were able to design a cuff to get the desired flow.”
Designing the perfect cuff
However, once they had determined the particular shape of the cuff, a new problem emerged: how to translate that shape from a flat patch material and form it into the cuff. For help, Hoganson turned to his partners at Dassault. With assistance from one of their aerospace engineers, Hoganson and his team used a very complex software developed for airplane wing engineering to “unfold” the cuff on the computer and generate the shape necessary to recreate the cuff from a patch material.
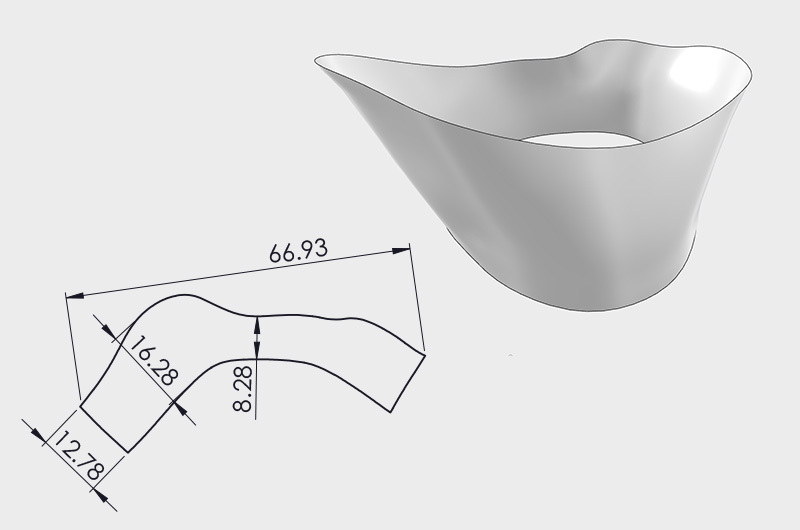
“The whole process took a few weeks, as we made some improvements in the design,” says Hoganson. It also gave the team time to allow one of their own engineers, Noah Schulz, to learn the process. “It was only possible because Dassault had developed this tool that involved highly complex math that designed how to patch wings using the stretchiness of the mechanical properties of the wing patch materials, which we could then use to incorporate the stretchiness of the aortic patch materials. We were grateful that they were willing to share this software and their expertise with us.”
When it came time for surgery, the outcome was phenomenal. While Hoganson was performing the surgery, a couple of the team’s engineers were observing the procedure virtually, as they routinely do, checking computer models and making sure everything was carried out precisely to plan. “The cuff fit exactly as it was supposed to,” says Hoganson. “When we removed the clamps and everything worked perfectly, it was really a bit of a moment for us all. Here was a very high-risk kid, and his outcome was great. It was a fun moment to see all that hard work turn out so well.”
A snapshot of the future
While this surgery was an exciting milestone in the development of these new technologies, Hoganson sees it as one piece of a much larger effort. “It’s just a snapshot of what we’ve been doing and what we’re working towards,” he says. “We’re very excited about our continued collaboration with Dassault and applying these complex tools to make a measurable difference in our patients’ lives.
“Where appropriate, we’re trying to shift these efforts, and use these engineering tools to predict the best way to do surgery, and afterwards to see if they accurately predicted the outcome. Ultimately we want to understand how we can rely on these tools to help make better decisions for our patients.”
Hoganson says they are working towards applying the same workflow they used for this surgery to other surgeries they do more routinely. “Our team was recently funded to apply this technology to aortic patients in a clinical trial. Our plan is start with lower-risk arch patients and progressively apply to more complex arch patients,” he says. “As time goes on, we’ll do more cases using these new tools, while continuing to come up with creative solutions for patients who have more uncommon issues.”
Learn more about the Heart Center.
Related Posts :
-

Four things you should know about MAPCAs treatment
As the first grandchild in her family, Hannah Homan is in demand for frequent visits. She was also the focus ...
-

Treating MAPCAs with unifocalization surgery and cardiology care
Children born with a rare form of tetralogy of Fallot (ToF) face a challenging type of congenital heart ...
-

After surgeries to treat HLHS, Carter is healthy and happy at home in Florida
Carter Miller loves action. The 4-year-old Florida resident enjoys riding on golf carts and flying high on swing sets. ...
-

Advancing global health: Using AI to detect heart disease in children
In many low- and middle-income countries, pediatric cardiologists can’t help children with congenital heart conditions because of a critical ...





