Adam takes a pause from his active life for non-ossifying fibroma

Adam was 11 in early 2024 when he and his bike slid under a downed tree. Such events aren’t unusual for Adam, who finds plenty of opportunities to test the limits of gravity near his home in Southern Maine. “Adam is the epitome of activity,” says his mother, Jessica.
After the bike incident, however, he noticed a bump on his right shin. He and his parents would learn that the bump was not related to the accident, but at the time, they only knew it was increasingly painful. “It was getting hard to walk,” says Adam.
An orthopedic surgeon in South Portland ordered an X-ray, and when the images came back, he ordered an MRI. Things snowballed from there.
A very large tumor
“The lesion was massive,” says Jessica. Embedded in Adam’s tibia (the larger of two bones in the shin), was a large mass. “It was essentially as thick as the bone from front to back and side to side,” says Jessica.

Adam’s doctor in Portland recommended Dr. Megan Anderson of the Bone and Soft Tissue Tumors Program at Boston Children’s Hospital. “He felt Adam needed someone with Dr. Anderson’s expertise,” says Jessica.
Within a week, Adam and his parents were meeting with Dr. Anderson. To save time and a drive to Boston, they met with her virtually. Having reviewed the images of Adam’s tibia, she told them she believed the mass was a non-cancerous bone tumor called a non-ossifying fibroma.
This was the good news. Non-ossifying fibromas are relatively common in growing children, particularly boys. Most non-ossifying fibromas go away without treatment, often before anyone realizes they were even there.
The bad news was that Adam’s tumor was so large, it had weakened the bone around it. Dr. Anderson compared the strength of Adam’s tibia to that of an eggshell. The bone could easily break, and if it did, repairing it would require extensive surgery. She recommended an operation to remove the tumor before that happened.
The news was alarming, but Jessica felt reassured by Dr. Anderson’s 20 years of experience treating bone and soft tissue tumors. “There was just a sense of confidence with her,” recalls Jessica. This helped Jessica remain positive for Adam, as did a family member’s advice to, “assume it’s benign until proven otherwise.”

Hello Boston, goodbye tumor
Adam’s first in-person visit to Boston Children’s took place in early June, on the day of his surgery.
In the operating room, Dr. Anderson performed a procedure called curettage to remove the tumor. She then filled the gap with bone graft to stimulate Adam’s natural healing process to create new bone. She also confirmed that the tumor was a non-ossifying fibroma.
Later that same day, Adam walked out of the hospital on crutches and returned to Maine with his parents. “My main goal was, do not stay the night at the hospital,” he says. “I wanted to sleep in my own bed.”
From non-weight bearing to wake surfing
Unfortunately for anyone who’s happiest in motion, bone healing means sitting still. As his recovery wore on, Adam grew restless. He wanted to go wake surfing by the end of the summer, and with signs of fall moving in, that desire loomed ever larger.
While Adam felt ready to get moving again, Jessica was concerned. Then, during a follow-up visit in August, Dr. Anderson told them that Adam’s healing was “exceptional.” Encouraged, Adam showed her videos of wake surfing and explained why it would put far less pressure on his leg than water skiing. To his delight, Dr. Anderson said his leg appeared strong enough to give it a try.

Soon after that conversation, Adam was out on the water. “I got right up on the first try,” he reports. “It didn’t hurt at all!”
Whooping it up in winter
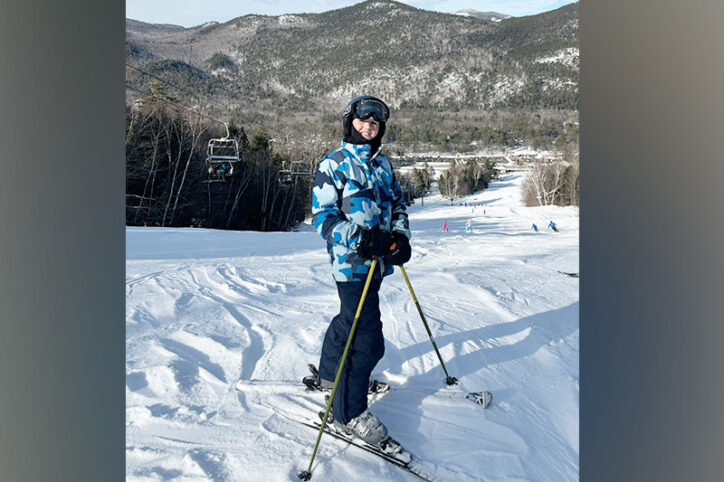
Though he missed the first half of the fall soccer season, Adam was back on the field by the time his team made the championships. By winter, he was truly back: ice fishing and zipping past his parents on skis. “I do like, 45 miles an hour down the trails. She only goes 15,” he says, gesturing at his mother.
“I don’t know if that’s accurate,” laughs Jessica. But she and Adam agree that within six months, he could do everything he’d been doing before surgery.
They also agree that they’re happy they sought care at Boston Children’s.
“I felt supported, I felt guided in a scary situation,” says Jessica. “Adam had absolutely the best care that I could have ever hoped for.”
“It was amazing,” says Adam.
Learn more about the Bone and Soft Tissue Tumors Program.
Related Posts :
-

Bone cancer surgery: A difficult choice
Nolan and Natasha might never have met if they hadn’t been diagnosed with bone cancer. Nolan, 13, is a natural ...
-

Generations of excellence in caring for childhood bone cancers: Dr. Gebhardt and Dr. Anderson
When Dr. Mark Gebhardt was a surgical resident at Boston Children’s Hospital in the early ’80s, doctors were just ...
-

Hard and beautiful at the same time: Five lessons of raising a medically complex child
When they learned they were expecting a baby, Michelle and Stephen Strickland were delighted. The South Carolina couple looked forward ...
-

3D imaging could become standard practice in orthopedics. Here’s how.
It took a trained eye to see the abnormality on the patient’s X-ray. There, hidden behind the acetabulum was ...





