AI could change the way we look at hip preservation
Orthopedic surgeons and biomedical engineers are trained to approach adolescent and young adult hip pain from two different perspectives. Surgeons typically look at conditions such as femoroacetabular impingement (FAI) and hip dysplasia from a clinical point of view. Engineers more often focus on the technology angle.
These two perspectives have come together at Boston Children’s Hospital, resulting in a tool that could improve diagnosis and clinical planning for hip patients around the globe.
Two decades of hip data made accessible with AI
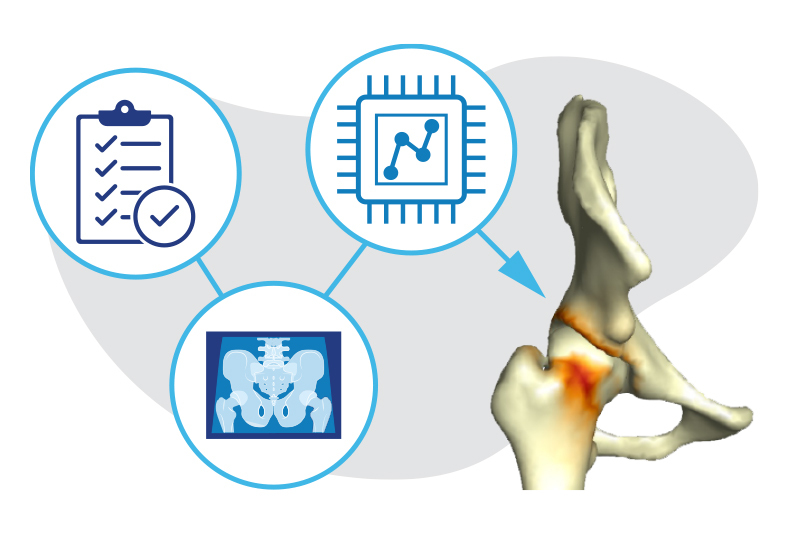
VirtualHip is a software platform that uses artificial intelligence (AI) and 3D imaging to support diagnosis and treatment of pediatric hip deformities. The idea grew out of conversations between Dr. Ata Kiapour, director of Boston Children’s Musculoskeletal Informatics Group, and Dr. Young-Jo Kim, director of the Child and Adult Hip Preservation Program, that began in 2017.
“I started shadowing the surgeons on the hip preservation team to understand how they worked and how technology might help,” says Kiapour. In doing so, he found an unmet clinical need for personalized diagnosis and treatment planning. He also discovered a largely untapped source of data: images and clinical notes on more than 10,000 hip patients from the past 20 years.
Our goal is to provide detailed information so surgeons can plan the best treatment for each patient.”
The potential of such data is comparable to a physician who has treated thousands of hip deformities and remembers them all in detail, says Kiapour. “That physician can look at a patient’s clinical profile and tell you, ‘We have treated patients like this and found that this approach works best.’”
But because the historical patient data wasn’t searchable, it was largely inaccessible. To unlock its potential, VirtualHip uses AI to process historical clinical records and match current patients with past patients with similar clinical profiles. These historic, deidentified patient records will provide important insights as surgeons diagnose and plan treatments for their current patients. That’s one aspect of VirtualHip. The other aspect involves comprehensive 3D image analysis.
The combined power of AI and 3D modeling
To diagnose hip deformities, orthopedic surgeons typically rely on a physical exam and diagnostic imaging. While some hip deformities are easily visible through MRI or CT scanning, many are not. Further, the impact of some hip deformities often depends on the position of the hip. In the case of FAI, for instance, a hip may only be painful when in motion and the bones rub together.
The limitations of traditional diagnostic imaging also complicate treatment decisions. Could physical therapy resolve the issue, or does the patient need surgery? In the case of impingement, how much bone needs to be removed for the hip to move freely without pain? In the case of dysplasia, at what angle should the surgeon rotate the acetabulum (hip socket) so the femoral head fits securely in the socket?
VirtualHip uses MRI or CT imaging to create a 3D model of the hip joint and then uses this model to automatically generate a comprehensive set of measurements of the hip’s structure. This data, combined with information from the clinical exam, provides a comprehensive view of the hip and areas of impingement or instability. Surgeons will be able to pinpoint the location and severity of the deformity with a level of accuracy not possible today.
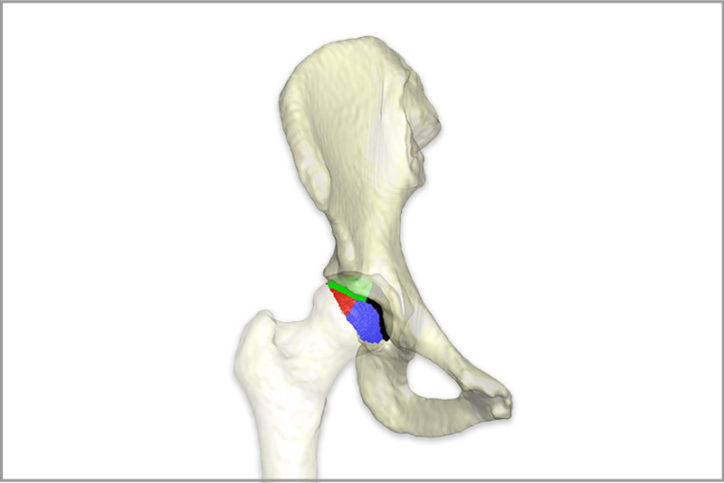
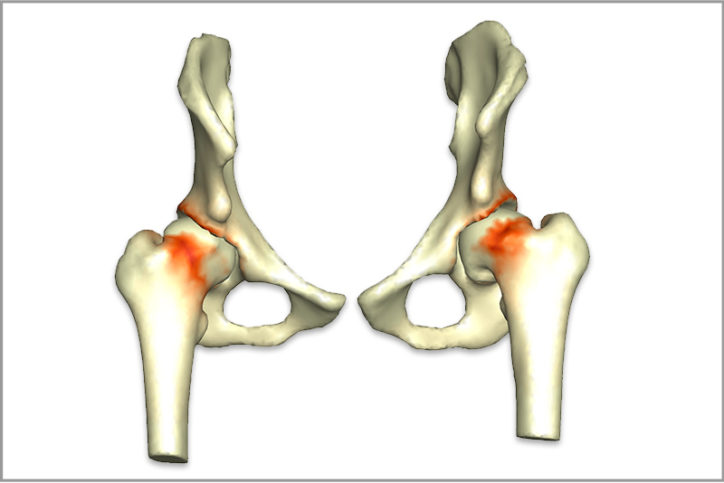
“Once you have a 3D model, you will be able to ask the software to simulate the full range of motion,” explains Kiapour. “These are the complex patterns that are not obvious on 2D images.”
With a detailed analysis of the hip’s structure and range of motion, VirtualHip will match the analysis with comparable historic patient data to provide information on outcomes associated with various treatment approaches. Such detailed knowledge could help improve the precision of hip preservation procedures, helping surgeons avoid over- or under-corrections. “Our goal is to provide detailed information so surgeons can plan the best treatment for each patient,” says Kiapour.
A unique collaboration and a promising future
Kiapour points out that VirtualHip is not the first platform to analyze hip impingement, but that it offers unique capabilities, including the automatic generation of detailed measurements without relying on a technician. It can also assess a patient’s risk of impingement or instability across a wide range of motion and process historic patient data to provide personalized analysis and treatment suggestions.
The insights that inform the development and refinement of these and other capabilities grew out of an ongoing collaboration between Boston Children’s orthopedic surgeons, radiologists, and engineers. For five years and counting, Kiapour and his team have worked closely with Dr. Kim and Dr. Eduardo Novais from the hip preservation team and Dr. Sarah Bixby from Radiology.
We are blessed to work in an environment where multidisciplinary collaboration is highly encouraged, and clinicians are eager to participate in translation research.”
“Clinicians are the end users for this platform, so keeping them in the loop during development is necessary to ensure the platform will address their needs,” says Kiapour. Working together, the team has developed a technically sound platform that provides clinically relevant information in a clinician-friendly format. “We are blessed to work in an environment where multidisciplinary collaboration is highly encouraged, and clinicians are eager to participate in translation research.”
The combined team continues to develop and validate the prototype so that it can be used in a clinical setting. The ultimate goal is to make VirtualHip available for widespread use in hip treatment centers. The project could also herald a new use for data science in pediatric orthopedic care: using AI to make the lessons of historical patient data accessible to surgeons as they plan their patients’ care.
Learn more about the Child and Young Adult Hip Preservation Program and the Musculoskeletal Informatics Group.
Related Posts :
-

The surprisingly specific genetics of joint disease
A new study provides unexpected insights into the biology of two common, heritable orthopedic conditions: developmental dysplasia of the hip (...
-

Always an athlete: Drew and Legg-Calve-Perthes disease
When he looks back on the diagnosis that forced him to stop playing sports entirely for more than a year, 11...
-

After hip dysplasia, Emma smashes her cast
When she could walk again, Emma Wilkinson and her parents threw a big party. Diagnosed with hip dysplasia at the ...
-

Printing a plan to resolve an athlete’s pain
Just days away from a complex hip surgery, Louise Atadja smiles and laughs. “I’m not really nervous at all. ...