Teaming up to fast track a novel gene therapy for Diamond-Blackfan anemia

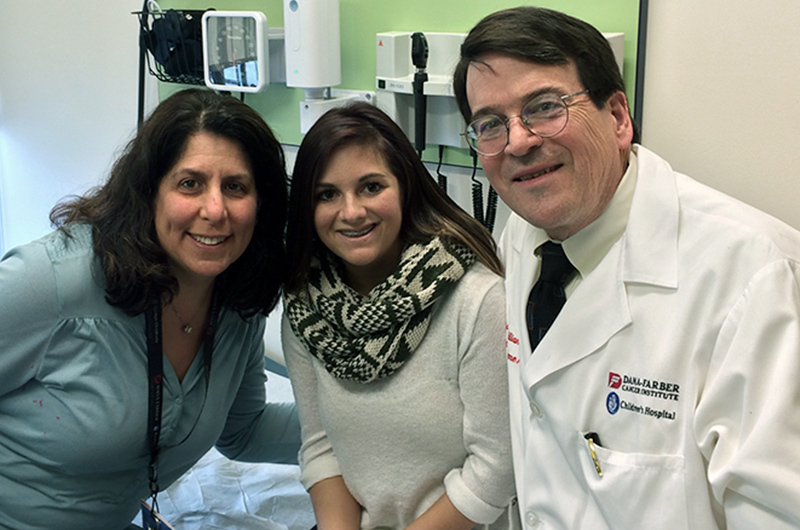
Looking at Lindsay Krieg, it’s impossible to tell she has spent her entire 29 years in an out of hospitals managing a rare blood disorder. “It’s routine for me,” she says. “It’s all I’ve ever known.”
Diamond-Blackfan anemia (DBA) prevents Lindsay’s bone marrow from producing the red blood cells essential for carrying oxygen from her lungs to the rest of her body. To replenish her red blood cell supply, she requires monthly transfusions. And with each transfusion iron accumulates in her bloodstream. If the iron is not removed, it can lead to heart and liver failure, so she is routinely evaluated at Dana-Farber/Boston Children’s Cancer and Blood Disorders Center and follows an iron chelation regimen.
Currently, the only curative treatment for DBA is a bone marrow transplant but only if a well-matched donor can be found. Still, that carries with it its own set of risks and complications. Fortunately for Lindsay, she’s been able to stay healthy without one.
A deeper understanding of DBA
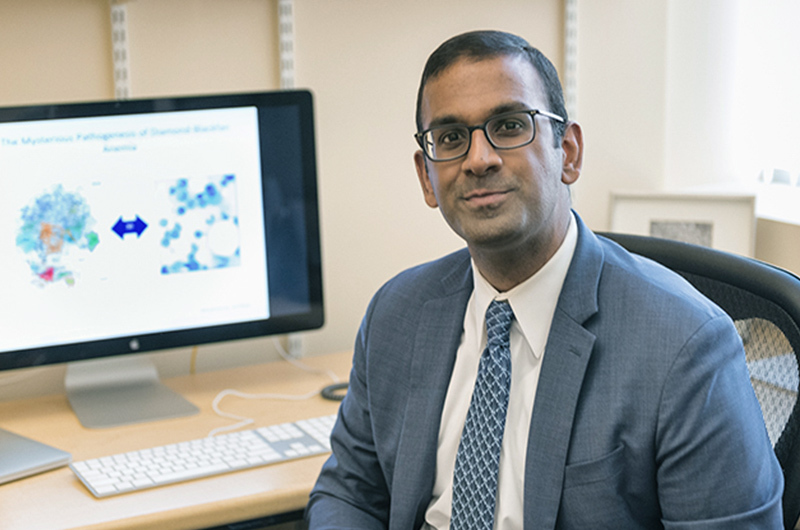
The lack of a cure or a sustainable long-term solution for people with DBA, like Lindsay, is what inspired hematologist Vijay Sankaran, MD, PhD, to begin experimenting with potential treatments, specifically gene therapy. The problem is DBA is not caused by one gene mutation but rather 26 (at least), ruling out the traditional gene therapy approach involving the replacement of a defective gene.
What Sankaran and his colleagues showed in a series of papers over the last few years is that the genes associated with DBA all provide instructions for making ribosomal proteins — components of cellular structures called ribosomes, the protein builders of the cell. And, these ribosomal protein mutations effect how the GATA1 protein, critical in the development of red blood cells, is produced.
“So, this is a downstream consequence of all these mutations,” says Sankaran. “And knowing this, we have shown — at least in preliminary studies with lentiviral vectors — that if we reintroduce GATA1, even in the setting of these mutations, we can actually rescue the phenotype, we can rescue the ability of the cell to undergo a thorough differentiation and enable full maturation of the cells.”
The challenge is regulating GATA1’s expression. Sankaran refers to it as the “Goldilocks effect.” Just as Goldilocks sought porridge that was “just right,” Sankaran’s lab has been working on targeting the “just right” levels of GATA1 expression to regulate red blood cell production. They identified what elements turned GATA1 on or off.
“I think the promise here, and the real excitement is we have the possibility of creating a gene therapy vector. Now, how do we translate that into a treatment for patients?”
Bringing promising treatments to patients by way of D3A
The translation of discoveries in the laboratory into potential treatments for a condition like DBA is challenging. Sankaran’s expertise is understanding blood disorders at a fundamental level but not necessarily the mechanisms to translate his research to patient care.
Enter D3A.
D3A, otherwise known as the Drug, Device and Diagnostic Accelerator Program, is a Boston Children’s Hospital program led by William Clarke, MD, D3A faculty director, and Mei-Mei Huang, PhD, D3A program manager. D3A is designed to identify innovation at Boston Children’s that would benefit from expert advice, additional investment, solid program management, and external technical resources to help faculty fast track ideas into full-scale development.
“We have the full project plan, we have the manufacturing plan, and we have the regulatory plan — all of which is relatively in the weeds but incredibly important,” says Clarke. “Faculty members will often say, ‘We didn’t know how to do this.’ Well, that’s why we’re here. Mei-Mei and I spent a long time in industry learning how to do this.”
D3A is not only acting as a guide but also providing vital and valuable resources. Clarke and his team connected Sankaran with the resources and connections to manufacture the DBA vector in a scale that can be tested in Sankaran’s preclinical models.
“I think what a patient cares about is not whether we have an advance that might help them but an advance that can change lives,” Sankaran says.
That’s the chasm D3A seeks to fulfill. And it’s Sankaran’s hope in the next couple of years, he can move from what’s an interesting observation in the lab to actually translating that to people like Lindsay, who have dealt with DBA their whole life.
Although Lindsay admits she doesn’t know a lot about gene therapy, she says if it is safe and effective, she would consider it in the future. But for now, she is focused on more than just managing her DBA. She has a September wedding to plan. “I’m just living my life,” she says.
Learn more about the Gene Therapy Program.
Related Posts :
-

The dopamine reset: Restoring what’s missing in AADC deficiency
In March 2023, a young girl came to Boston Children’s Hospital unable to hold up her head — one striking symptom ...
-

Tough cookie: Steroid therapy helps Alessandra thrive with Diamond-Blackfan anemia
Two-year-old Alessandra is many things. She’s sweet, happy, curious, and, according to her parents, Ralph and Irma, a budding ...
-

Blood across our lifetimes: An age-specific ‘atlas’ tells a dynamic story
The stem cells that form our blood, also known as hematopoietic stem cells (HSCs), are with us throughout our lives. ...
-

A small act of kindness: Blood donations get Sadie off the sidelines after her aplastic anemia diagnosis
In March of 2024, Sadie’s life was interrupted. A busy high school senior with classes to attend, soccer matches to ...