Cerebral adrenoleukodystrophy: How the Cooksons dodged a devastating disease

Heather Cookson believes that if she hadn’t insisted her son Ricky get a brain MRI to investigate his frequent headaches, neither he nor his younger brother Jerry would be walking or living full lives today.
“I just wanted peace of mind,” she says. “Ricky got the MRI, and that’s when the lesion was found.”
The MRI showed damage to the white matter in Ricky’s brain. That led to genetic testing, and at age 8, Ricky was diagnosed with cerebral adrenoleukodystrophy (CALD), a devastating disorder in which boys progressively lose neurologic function.
CALD is caused by mutations in the ABCD1 gene that prevent the body from breaking down very-long-chain fatty acids. The fatty acids build up, damaging the brain and nervous system. While Ricky wasn’t yet showing symptoms besides headaches, most boys with CALD eventually become unresponsive if untreated and pass away within a decade.
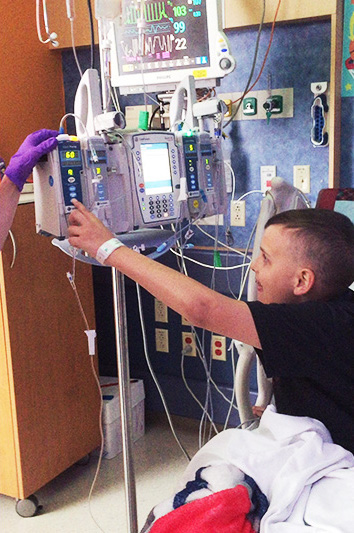
That’s all Heather needed to hear. Six weeks later, Ricky was an inpatient at Boston Children’s Hospital.
“You want to treat boys as early as you possibly can,” says his physician, Dr. Christine Duncan, medical director of clinical research and clinical development for Boston Children’s Gene Therapy Program and a senior physician with the Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. “If you treat it late, it doesn’t work.”
Ricky’s stem cell transplant
At the time, the only available treatment was a blood stem cell transplant, a lengthy and risky procedure. It can be curative, but it requires finding a genetically matched donor to avoid a life-threatening complication: graft-versus-host disease (GVHD), in which cells from the donor attack the recipient.
Jerry would have been a perfect donor match for Ricky — but that’s when the family learned that Jerry, too, had the CALD mutation. While Jerry’s health was monitored, Ricky got a stem cell transplant from an unrelated cord blood donor.
Ricky was spared from GVHD. But the strong immunosuppressive drugs he received to prevent it put him at high risk for infections, requiring him to quarantine for a year.
“The only buildings he could go into were our house and the hospital,” says Heather. “We couldn’t go to a restaurant or have Thanksgiving with our family. But we made it work.”
“I had a long recovery; I couldn’t do anything,” Ricky says. “Once the first year went by, things started going back to normal.”
Jerry’s gene therapy treatment
Several years later, Jerry’s CALD, which had been silent, was becoming active. A new treatment had recently become available: gene therapy using patients’ own cells.
It was perfect timing: Jerry received the gene therapy, now approved by the FDA and called SKYSONA, through a clinical trial. Dr. Duncan and Dr. David A. Williams explain it here:
The therapy replaces the mutated ABCD gene with a healthy copy. The Cooksons decided to try it, knowing that Jerry could still have a stem cell transplant as a “plan B” if the gene therapy failed.
“If there wasn’t a plan B, he could have lost his speech, his mobility, or possibly even passed away, which is something unthinkable,” says Heather.
The odds were in his favor. In a six-year follow-up study just published, 81 percent of 67 treated boys were alive and free of six severe disabilities: blindness, loss of the ability to communicate, need for tube feeding, wheelchair dependence, complete incontinence, and complete loss of voluntary movement. Ninety-four percent have had no decline in neurologic functioning.
The family knew that the gene therapy carried a risk for cancer, confirmed in another study co-led by Dr. Duncan. But Heather and Jerry appreciated gene therapy’s shorter recovery period of about three months.
Another big advantage: Because gene therapy used Jerry’s own cells — treating them in a lab and returning them through an IV infusion — it avoided the rigors of stem cell transplant and the need for a matched donor.
“Gene therapy involved more appointments in the beginning, but I thought it was a safer option,” says Jerry.
Monitoring long-term risks
Now 19 and seven years out from his gene therapy, Jerry is doing well, working as a food delivery driver until he starts college next spring. Ricky, now 21 and 12 years out from his stem cell transplant, is also well and currently looking for work, hoping to get a job in IT.
Neither especially wants to talk about CALD or their treatments. “They just want to put it on the back burner and live their lives,” says Heather.
Because of the cancer risk, Dr. Duncan monitors Jerry with checkups every few months. Should a cancer develop, he would need to be treated with a stem cell transplant. Ten percent of boys developed cancers in the recent study, primarily a type called myelodysplastic syndrome (MDS). Four of the seven boys recovered after a stem cell transplant, one passed away from GVHD, and two are still receiving cancer treatment.
While scientists at Boston Children’s and elsewhere investigate ways to make both stem cell transplant and CALD gene therapy safer, Dr. Duncan works closely with families to help them understand the risks and benefits of both. “CALD is an awful disease,” she says. “It’s so critical that these boys have options.”
She outlines the options in detail in this hour-long town hall:
Disclosure: Dr. Duncan is a consultant for bluebird bio, which funded the gene therapy studies.
Related Posts :
-

Gene therapy for adrenoleukodystrophy: Studies find both risks and benefits
Cerebral adrenoleukodystrophy (CALD), portrayed in the film Lorenzo’s Oil, is a devastating disorder caused by a mutation on the ...
-

Making history: Gene therapy for CCALD gives Conner a second chance
Like a lot of 6-year-olds, Conner Hess finds joy in simple acts: drawing pictures, cuddling his two cats, and playing ...
-

A big step toward curbing graft-vs.-host disease after bone marrow transplant
A drug used for rheumatoid arthritis has moved a step closer to FDA approval for a desperately needed new use. ...
-

In a thriving gene therapy program, nursing leadership is the driving force
Gene therapy was made possible by decades of technological advances. But to execute gene therapy at scale? That would not ...





