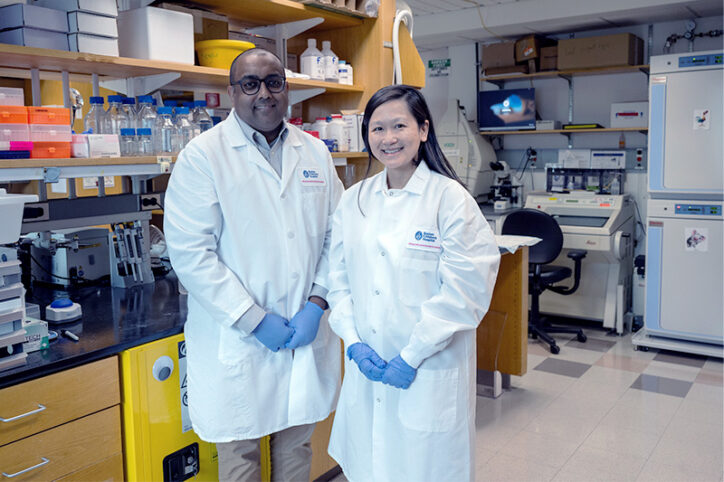
Two rising stars in kidney genetics: Nina Mann and Amar Majmundar

A healthy, functional kidney must maintain a delicate balance of water, nutrients, and electrolytes so it can properly filter the blood and produce urine. That often makes caring for patients with kidney disease an exercise in chemistry and mathematics — an aspect of nephrology that attracted two young physician-scientists.
Coming from different paths, Nina Mann, MD, and Amar Majmundar, MD, PhD, met during their nephrology fellowship at Boston Children’s Hospital, working together in the clinic and in the kidney genetics lab of Nephrology Division Chief, Friedhelm Hildebrandt, MD. In 2022, with Hildebrandt’s support, they established and became co-directors of the Kidney Genetics Clinic — one of very few in the country at a children’s hospital.
Together with genetic counselor Bree Martin, MS, LCGC, they work with families to find genetic diagnoses for children with rare kidney disorders and develop custom care plans.
“We had research experience evaluating genetic testing results in hundreds of kidney patients and wanted to bring that expertise into the clinical environment,” says Majmundar.
Nephrology and numbers

Initially, Majmundar was drawn to genetics through research experiences in college and during his PhD thesis. But as a resident at Boston Children’s, he helped care for a patient in the ICU who needed dialysis after a bone marrow transplant and worked closely with nephrologists.
“I liked how they approached medical problems mathematically and their insights into the kids we were caring for,” he says. “Those questions might be a chore for some, but for me it was satisfying and interesting. It was really fun talking to our nephrologists about how to achieve better fluid and electrolyte balances for our patients and how best to approach dialysis. I felt I fit in with the folks who were doing nephrology.”
He was also struck by the case of a child with cystinosis, a genetic kidney disorder. “Electrolyte abnormalities were not allowing him to grow well,” he says. “We had to figure out why that was happening and calculate how to get things back to a normal balance. Nephrology is a great field for people comfortable with problem solving.”
Mann’s path was more circuitous. She started out studying chemical engineering at MIT, but became interested in clinical medicine. In medical school, she initially felt drawn to cardiology: the quantitative nature of cardiac physiology appealed to her engineering side. During her pediatrics residency, she also became interested in genetics, particularly after seeing the potential of new genomic technologies for diagnosis and personalized therapy.
During her residency at Boston Children’s, a conversation with Sam Lux, MD, changed Mann’s trajectory. Lux, former chief of Hematology/Oncology and renowned for his mentorship, gave her several leads to further explore her interest in genetics. One led her to Hildebrandt’s lab.
“I quickly realized that nephrology is a very quantitative field. There is a lot of math involved in calculating dialysis prescriptions or in understanding how the kidneys are handling the salts in the body,” she says. “I also enjoyed the long-term relationships that nephrologists have with their patients and families.”
A research approach to kidney disease
Through their training, Mann and Majmundar bring complementary expertise and research interests into the Kidney Genetics Clinic.
Mann has studied the genetics of chronic kidney disease, congenital anomalies of the kidney and urinary tract, and bladder dysfunction. She currently spends part of her time with the Department of Urology’s CHEER clinic studying the genetics of nocturnal enuresis (bedwetting) and voiding dysfunction.
“I became interested in how people achieve continence, which is actually a rather complex biological process,” she says. “Voiding dysfunction often runs in families and carries with it a lot of stigma. It can have a significant impact on a child’s quality of life and if very severe, can impact kidney function as well.”
Separately, Mann is using cellular models and proteomic approaches to understand how mutations in a single gene, WT1, cause kidney failure.
The Majmundar lab is focused on finding genetic causes of nephrotic syndrome, a hard-to-treat condition that can quickly cause kidney failure. He has found that certain mutations, like those he identified in the genes NOS1AP and TRIM8, disrupt the structure and signaling inside the kidney’s filtering cells, or podocytes. By modeling the mutations in cells and mice, he hopes to discover approaches that will improve podocyte and kidney function.
In collaboration with Michelle Baum, MD, of the Kidney Stone Program, Majmundar is also doing genetic studies in children with kidney stone disease. Most recently, he identified mutations in the gene OXGR1 and received a grant to study its effects in mouse models.
Preventing kidney failure through targeted treatments
Both Mann and Majmundar enjoy the mix of research and clinical care in their work. On a given day they might see patients in the morning and work on lab models to study the mechanisms of their disease in the afternoon. As they encounter children with different genetic mutations, they invite them to join patient registries to better characterize each disorder.
Ultimately, they hope to discover and test treatments based on the cellular and molecular pathways affected by the genetic mutations. “I think targeted therapies are the future with various forms of gene therapy already being developed for other types of genetic diseases,” Mann says.
Of greatest interest are treatments that might address more than one form of kidney disease.
“There may be a hundred genetic causes that coalesce into a smaller number of pathways that affect kidney function,” Majmundar says. “As we get more information on root causes, we hope to treat patients at an earlier point in their disease. We want to focus on areas where we can make a big impact.”
Learn more about the Kidney Genetics Clinic.
Related Posts :
-

A master regulator of kidney health?
End-stage kidney disease often begins with injury to podocytes. These highly specialized cells are a critical part of the glomeruli, ...
-

If your baby or toddler needs peritoneal dialysis: Tips for parents
Marybeth Bentson and Theresa Pak have helped a lot of families cope with childhood kidney disease. As long-time nurses in ...
-

First-of-its-kind clinical trial aims to improve outcomes in pediatric transplant patients
For the last 20 years, pediatric kidney transplant patients have been treated with the same immunosuppressive medication combinations and have been ...
-

Unstoppable: Cairo’s journey for kidney care began even before birth
Like lots of babies, Cairo Carter was born screaming — and his parents were thrilled. “We just wanted him to scream ...