Robotics, spinal fusion, and the quest for 100 percent accuracy

In any spinal fusion surgery, accurate screw placement is a top priority, and for good reason. Incorrectly positioned screws are the number one cause of surgical complications and revision surgeries according to the Scoliosis Research Society. While the vast majority of malpositioned screws — between four and 15 percent of all screws placed — do not have clinically significant consequences, the goal for many spine centers is zero.
“If you’re searching for perfection, you’re looking for ways to maintain 100 percent accuracy,” says Daniel Hedequist, MD, chief of the Spine Division at Boston Children’s Hospital.
In 2019, Boston Children’s became one of the first pediatric spine centers to adopt the Mazor X Stealth robotic guidance system. The system combines pre-operative planning, robotic guidance, and surgical navigation. Hedequist sees the use of a guidance system as an important step in the ongoing evolution of technologies that, when harnessed with care, are moving the field toward ever-greater accuracy and safety.
“With some patients’ anatomies, it’s easy to find a clear trajectory, but if the patient is small or has a severe deformity, it can be much more difficult,” says Hedequist. “The robot has no idea if a trajectory is easy or difficult. Thanks to pre-surgical planning and navigation, it sets the path and the surgeon can drill with greater confidence.”
Since introducing a guidance system into its surgical suite, the Spine Division’s four surgeons have used it in more than 300 spinal fusion surgeries. In that time, Hedequist and his colleagues have closely monitored the outcomes of cases, identified areas of potential errors, and refined their processes and technology to optimize safety. Their observations, published in the Journal of Pediatric Orthopedics and numerous other publications, provide valuable insights for any spine center using or considering robotic guidance.
Workflow modifications to increase accuracy
Registration of the patient’s anatomy (matching the position and angle of the vertebrae to the navigation software) is essential to robotic guidance safety. Loss of registration can occur for many different reasons. For this reason, Boston Children’s surgeons double check registration accuracy before drilling each pilot hole and again before placing each individual screw.
In a review of 88 operations using the robot between February 2021 and November 2021, loss of registration was detected and corrected in six of the first 35 procedures. Hedequist concluded that screw placement could create enough torque to shift adjacent vertebrae.
The team changed its surgical process once they’d identified this potential issue, drilling all of the pilot holes before placing the screws. With this procedure implemented, there was no further loss of registration in the remaining 53 patients.
Technology to increase accuracy
One of the early concerns with the robotic navigation system was the low speed of the navigated drill and its potential to slip on uneven or sloping surfaces. This issue, known as skiving, could skew the starting point, the angle of the drill path, or both.
Emerging technology: Surgical headset
Computer-assisted navigation gives surgeons a new level of visibility, but there is a tradeoff. In crowded operating areas, the navigation screen is often positioned to the side, forcing surgeons to look away from the surgical area. Surgeons at Boston Children’s have started using a headset during navigated freehand procedures that allows them to see both the patient and the navigation screen simultaneously.
Early on, Boston Children’s surgeons mitigated the risk of skiving by flattening any sloping or irregular surfaces before drilling. Doing so reduced the risk of slippage but could interfere with registration if vertebrae shifted in the process.
A navigated high-speed drill capable of cutting a direct path through irregular surfaces made it unnecessary to flatten out bony surfaces. Boston Children’s is the first pediatric center to use the high-speed drill. The surgeons further ensure safety with a “tapping” method, which allows them to feel the drill moving down the pedicle and into the vertebral body.
Moving toward 100 percent accuracy in spinal fusion surgery
Soon after adopting the guidance system, Boston Children’s Spine Division recruited other centers using the system to participate in a registry of pediatric spine centers around the country. Participating clinicians and researchers are using the pooled outcomes data to analyze the system’s long-term impact on accuracy, the length of operations, and radiation exposure.
“Technology will continue to play an integral role in driving accuracy of spinal fusion,” says Hedequist. “As a highly experienced center that’s had success with freehand operations, we can help push the field forward without compromising safety.”
Learn more about the Spine Division.
Related Posts :
-

Generations of excellence in surgical care: Dr. Emans and Dr. Hogue
Some surgeons follow their patients for years, even decades. This is true of Dr. John Emans, who has treated patients ...
-

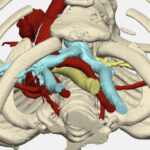
Reconstructing a chest wall, one virtual step at a time
It takes a village of clinicians and engineers to reconstruct a chest wall. It also takes a lot of 3D ...
-

Gracie’s complex spine
Halloween 2018 was no ordinary ghouls’ day for Gracie Neef. She and both her parents dressed up as the witches from “...
-

Saif looks ahead to life after spine surgery
Saif and his mother, Khawha Abbas, both had questions for Dr. Daniel Hedequist. For the past nine months, the family ...