Daphne’s story: Lifting the fog on bladder exstrophy
The day of their 18-week prenatal appointment was the first day of the most difficult 18 months of Pam and Jon’s life. When the ultrasound technician couldn’t see their baby’s bladder, they were sent home to try again later. They had so many questions, plus a 2-year-old daughter, their careers, and a house to take care of. Their beloved Red Sox were playing in the World Series. Family and friends offered, with the best of intentions, conflicting advice.
Pam panicked. Jon tried to stay calm.
A second ultrasound confirmed that their baby would be born with bladder exstrophy, a rare and complex birth defect where the bladder develops outside of the body. No one they knew had ever heard of bladder exstrophy, not even their obstetrician.
The year and a half that followed would be impossible and exhausting and triumphant. Ultimately, it would define a family and bring to light their love for each another and for life.
Amid the chaos, there were defining moments that, in retrospect, gave them clarity.
Talking to the MFCC
Pam and Jon were referred to the Boston Children’s Maternal Fetal Care Center (MFCC) and spent the next two weeks preparing for the visit. They read outcomes studies and research papers on bladder exstrophy — almost always authored by Dr. Joseph Borer, director of Boston Children’s Bladder Exstrophy Program. “We thought, ‘We’re going to know this man. This is going to be our guy,’” says Pam.
But two weeks felt long. “At that point, we were in imagination land because finding credible and detailed information on rare conditions is challenging,” says Pam. “I just wanted to speak to someone who knew what they were talking about.” Sitting at her desk at work, she received a call a nurse in the MFCC, confirming the upcoming appointment and offering to answer any questions. “It was so relieving to talk to someone who had seen this before and it wasn’t a total disaster,” says Pam. “She was very, very reassuring.”
Meeting Daphne
At Boston Children’s, Pam and Jon met with Borer and a host of other specialists. “Meeting Dr. Borer made me feel insanely better because he was just so calm and explained everything in ridiculous detail.” He answered questions and laid out the team’s treatment plan.
Daphne, meaning “victory,” was born in March. “Throughout the pregnancy, the only thing people would talk about was Daphne’s bladder,” says Pam. “I was just so excited to meet the little person attached to that bladder.” Daphne was the happiest baby, easy even. She was forgiving of her parents as they learned how to protect her exposed bladder during the 8 weeks leading up to her first major surgery. She smiled early.
As planned, Daphne underwent a 15-hour surgery called complete primary repair of exstrophy (CPRE). Orthopedic surgeon Dr. Young-Jo Kim also performed a procedure called a bilateral osteotomy to reform her pelvis. The hospital stay and follow-up home care were challenging, but things went as expected. For a while, at least.
Trusting their instincts
Two months post-surgery, Daphne started spiking erratic fevers and would go from perfectly happy to “disaster baby” — curled up in pain and screaming. The episodes got worse and more frequent.
People suggested Daphne was just being a fussy baby, but Pam and Jon knew something was terribly wrong. Repeated trips to the Emergency Department (ED) and to see Borer didn’t resolve the issue.
A month later, in the middle of the night, Daphne started throwing up and was lethargic. Pam and Jon rushed her to the ED, where an ultrasound revealed urine in Daphne’s abdomen. It turns out that Daphne was the only patient ever to have her urethra close after CPRE. With nowhere for the urine to go, her bladder had burst.
Borer showed up to the ED in the middle of the night, simply saying, “We’re going to fix this.” He repaired Daphne’s bladder and placed a catheter in her ureter to keep it dilated and allow urine to drain out.
Embracing the art of medicine
Unfortunately, the episodes continued after the surgery and were not the only complication, meaning at any moment for the next 6 months she could need emergency medical intervention to prevent further bladder or kidney damage. No matter the hour, if Daphne was in the ED, so was Borer. Sometimes, he would just sit with Pam and Jon for hours, thinking. “We knew Dr. Borer wasn’t going to stop until he figured out what was going on,” says Pam. “He was so focused on making things right.”
Jon adds, “It’s such a rare condition, and we were with the world’s expert. It was hard to see the end of it. We were just in survival mode.” The family’s trusted pediatrician, Dr. Shari Abramowitz, offered guidance. “There’s a point where medicine stops being a science and becomes an art,” she told them. Abramowitz believed that Daphne was in the hands of the only artist in the world who could find the resolution everyone was looking for. She helped Pam and Jon trust in Borer’s long-term vision and stay the course through Pam and Jon performing routine and emergency catheterizations at home, several hospital stays for emergency intravenous antibiotics and other surgical interventions.
Turning the corner
In April, shortly after Daphne turned 1, her urethra closed up again, but Borer was able to fix it before her bladder burst. This time, he made a slightly larger opening in her urethra— big enough to allow urine to drain but small enough to avoid continence issues down the road.
Things slowly got better after that. The episodes gradually got less severe and less frequent over the next year.
“The solution was a long time coming and it was difficult to navigate, but we got there,” says Pam. “It was hard to let go of panic mode because you never know when you are actually out of the woods, but we finally did.”
Enjoying a different kind of crazy
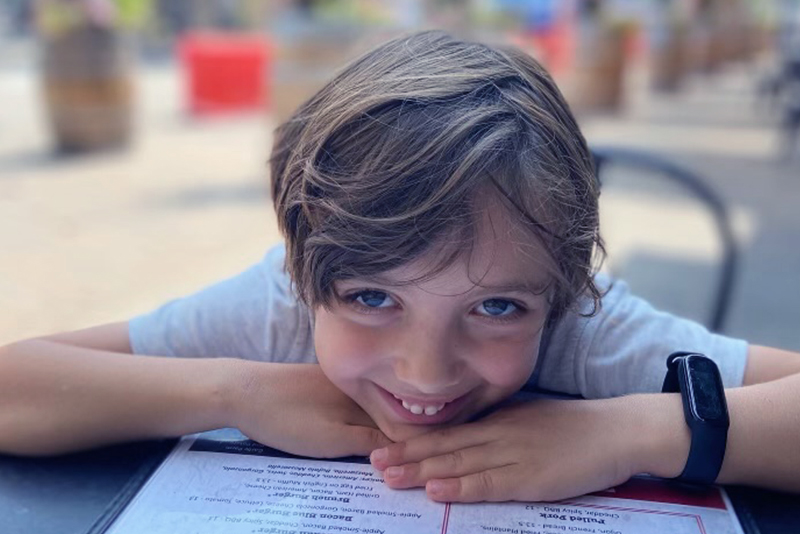
Now with three kids and a puppy (and still two careers and a house), life for Jon and Pam is “crazy” — in a good way. Daphne is a joyful and self-confident third grader with an incredibly sharp sense of humor. Her relationship to the condition has evolved as she has gotten older and taken on more of the day-to-day responsibility of managing it in new environments like schools and camps. “It’s been a lot of two-steps forward, and one-step back,” says Jon, “which can be challenging at times, but it hasn’t substantially impacted her social, academic, or extra-curricular experiences.”
“It’s easy to feel like this was about us and think, ‘why us?’ but this is not our story,” says Pam. “This is Daphne’s life,” adds Jon. “We’re just here to bridge the gap during a period of her life when she can’t manage things herself, and hand off that responsibility to her over time.”
Daphne loves playing baseball, soccer and basketball, hanging out with her friends, and writing her own comic strips, as well as spending time with big sister Hailey and little brother Theo, who was given the middle name of Joseph, after Borer. “There would be no Theo if Dr. Borer hadn’t found a solution when he did,” says Jon. “Our family wouldn’t be complete without him.”
Learn more about Boston Children’s Bladder Exstrophy Program.
Related Posts :
-

Henry's bladder exstrophy journey
Just a few months into his young life, Henry Packer has traveled from the Netherlands to Utah to Massachusetts — and ...
-



Henry's bladder exstrophy journey
Just a few months into his young life, Henry Packer has traveled from the Netherlands to Utah to Massachusetts — and ...
-


Jada’s story: After cloacal exstrophy repair, an unexpected gift
Koda Wilder Ladchuk was born slightly premature, healthy, and happy. But this isn’t just a story about 4-month-old Koda. ...
-


Stetson travels from Texas for bladder exstrophy care
As first-time parents, Rachael and Leroy Calk expected to have questions after their son, Stetson, was born. What they didn’...

