A ‘pump’ gene’s surprising role in early brain formation
In polymicrogyria, the cortex of the brain has many irregular, small folds (gyria) and disorganization of its layers. Many affected children have severe developmental delay, intellectual disabilities, and epilepsy, and many need to use a wheelchair. Mutations in several different genes can cause this “overfolding of the brain” condition.
Key takeaways
- The gene ATP1A3, associated with several neurologic diseases, is now found in polymicrogyria, in which the cortex has many irregular, small folds.
- It encodes a protein that makes up part of an ion pump, helping drive action potentials in neurons.
- Using single-cell RNA sequencing in tissues from developing human brains, researchers explored ATP1A3’s role in brain organization. They believe that ATP1A3 mutations may disrupt the balance of excitation and inhibition in the brain.
Studying four patients with polymicrogyria, Richard Smith, PhD, identified mutations in a gene that caused him to do a double-take. His curiosity drove him to investigate the role of this gene, called ATP1A3, in the developing brain.
“ATP1A3 is critical to many cell biological processes,” says Smith, an investigator the Division of Genetics and Genomics at Boston Children’s Hospital. “It’s one of the most important genes we have in our brains.”
Bio-electricity and brain development
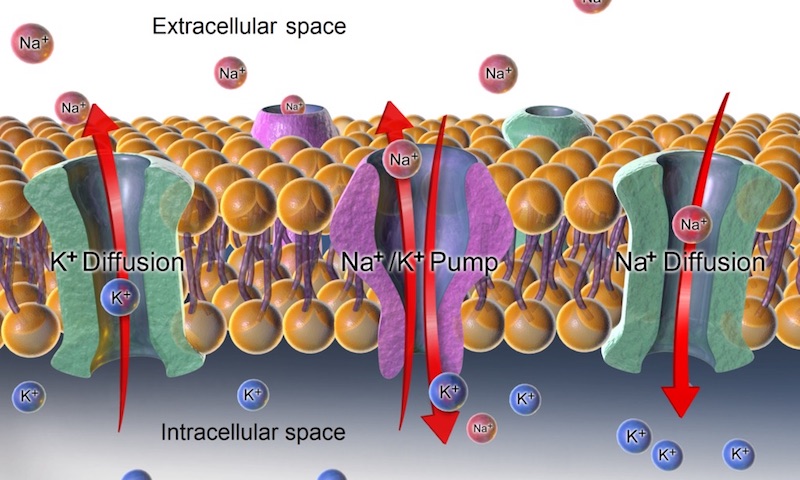
ATP1A3 encodes a protein that makes up part of a cellular pump. It moves sodium and potassium ions across the cell membrane, allowing our cells to maintain differing concentrations of charged ions on either side, similar to a battery. This difference enables electrical currents to flow into or out of cells, driving essential cell functions, including action potentials in neurons.
“For me it was very compelling to understand how these pump proteins, and the flow of ions, contribute to core mechanisms in brain development,” says Smith, an electrophysiologist by training. “We got a lot of great biological insights by studying these four patients.”
A spatial and temporal ‘atlas’ of ATP1A3
When and where in the typical developing brain is ATP1A3 turned on? To answer this question, Smith, with senior investigator Christopher Walsh, MD, PhD and colleagues at multiple other sites, obtained donated human tissues from several hospital tissue banks and the NIH NeuroBiobank. They analyzed samples from two times in early brain development: at around 20 weeks’ gestation, when the fetal cortex, initially smooth, starts to fold, and in infants soon after birth.
Using single-cell RNA sequencing (DropSeq) in collaboration with Marta Florio, PhD, at Harvard Medical School, they looked for expression (turning on) of ATP1A3 in about 125,000 individual neurons from 11 areas of the prenatal cortex. They also profiled about 52,000 neurons from the infants, sampling four areas of the cortex.
Overall, ATP1A3 expression levels were highest in the prefrontal cortex at both time points, and highest in the most active, frequently-firing neurons in the cortex. In the fetal cortex, ATP1A3 expression was particularly high in the subplate, a layer that disappears later in development. Electrical activity in the subplate is thought to be a hub of signaling driving synapse formation, neuron migration, and other brain developmental processes.
“In the infants, we found increased expression of the gene in interneurons, which are inhibitory,” says Smith. “We think that ATP1A3 mutations may disrupt the balance of excitation and inhibition in the brain, which could contribute to epilepsy in other ATP1A3-related conditions.”
Lessons for other ATP1A3-related diseases?
The work, published last week in PNAS, underscores how research in rare diseases can yield fundamental insights in biology — in this case, how the brain develops its contours and organizational pattern. It provides a map for future studies of how mutations in ATP1A3 cause the brain to form abnormally.
“When we published this as a preprint, a lot of people reached out to us with patients with overlapping phenotypes,” says Smith. “It is very exciting to better understand this disease.”
The findings may also inform scientists’ understanding of other known ATP1A3-related disorders. While the patients with polymicrogyria had severe mutations causing loss of function of the gene, milder mutations cause a spectrum of later-onset neurologic diseases. These include alternating hemiplegia of childhood, which causes bouts of temporary paralysis; a movement disorder known as rapid onset dystonia parkinsonism; and childhood-onset schizophrenia. These later-onset disorders may be more amenable to therapeutic intervention.
“Polymicrogyria is at the extreme end of severity, but we think that ATP1A3-related disorders in the ‘middle’ of this spectrum could have early pathogenic roots that might be treatable before they become more severe,” says Smith.
If newborn DNA sequencing becomes common, it could offer a window of opportunity for treating ATP1A3-related disorders before they manifest clinically, he adds.
And what about polymicrogyria? “A structural malformation is trickier to reverse, but infant brains are amazingly plastic and capable of reorganizing,” says Smith. “So if you could lessen the epilepsy-related damage from the earliest point, you could possibly improve quality of life.”
Smith is supported by the National Institute of Neurological Disorders and Stroke and the Tommy Fuss Foundation. Walsh is a HHMI Investigator, and receives funding from the Paul Allen Discovery Foundation and the NIH.
Learn more about Boston Children’s Division of Genetics and Genomics.
Related Posts :
-

New technique yields potential treatment for a common cause of autism
Since 2008, we have known that the 16p11.2 chromosomal region is linked with autism spectrum disorder (ASD). Now, researchers from Boston ...
-

‘Empowered to be there for Teagan’: New parents learn about hearing loss
Teagan O’Brien is a bright, spunky 4-year-old who loves reading, dancing, and playing outdoors. Her parents, Kim and Donnie, ...
-

Building better antibodies, curbing autoimmunity: New insights on B cells
When we’re vaccinated or exposed to an infection, our B cells spring into action, churning out antibodies that are ...
-

A journey through the intestine during colitis, cell by cell
Inflammatory bowel disease (IBD), causing devastating abdominal pain, persistent diarrhea, and rectal bleeding, is hard to control with current treatments. ...




