Five lessons learned from our Vaping Service
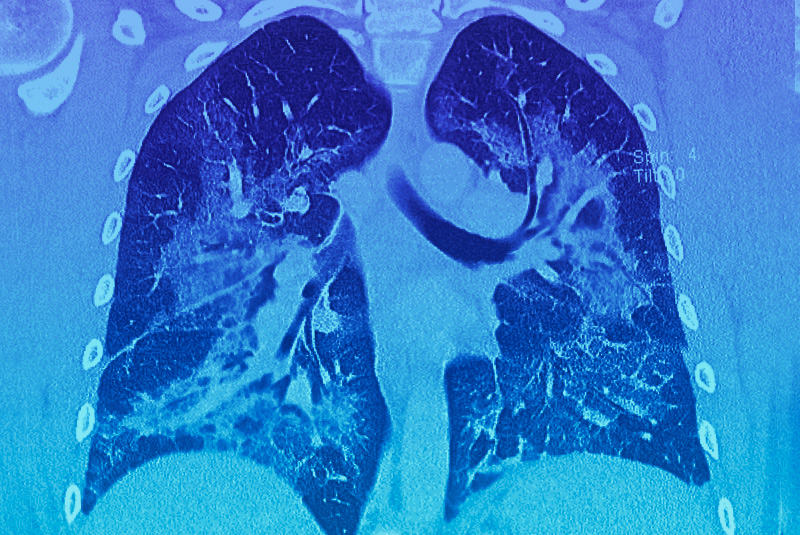
Vaping is a public health emergency in the United States. In recent months, over 2,000 people have become sick after using e-cigarettes and dozens have died. Yet despite the dangers involved, the number of young people who vape continues to climb, according to the latest Monitoring the Future study.
The Division of Pulmonary Medicine at Boston Children’s Hospital has responded to this crisis by creating a Vaping Service dedicated to caring for teens and young adults who are experiencing pulmonary-related effects from e-cigarettes. We have been able to leverage an array of resources to create a comprehensive response to this situation, according to Alicia Casey, MD, co-director of the Interstitial Lung Disease Program in the Division of Pulmonary Medicine at Boston Children’s.
Exploring lessons learned
Here are some of the top lessons we have learned from our Vaping Service that can help pulmonologists who work in pediatrics and adolescent medicine to strengthen their own efforts in this area:
- Since e-cigarettes can be very addictive, you need to treat both the health symptoms and also the underlying addiction.
“Due to the addictive nature of e-cigarettes, many people who have become ill from vaping — including those experiencing life-threatening effects — are unable to quit without significant help,” Casey says. That’s why our Vaping Service has developed a close partnership with experts from our Adolescent Substance Abuse Program (ASAP). When we have a patient with respiratory issues suspected to be related to vaping, it is imperative that they quit before their respiratory status worsens. We are fortunate to have direct access to high quality substance abuse treatment resources through Boston Children’s ASAP program. ASAP providers have educated our staff on how to identify patients who could benefit from their expertise. The ASAP program also works closely with the pulmonary service on triaging and evaluating patients who present with vaping-related respiratory complications.
2. When a patient presents with pulmonary symptoms, you need to know their vaping history to properly understand the risk for lung injury.
Since the signs of vaping-related pulmonary illnesses can look like the flu or pneumonia, pulmonologists must ask each patient if they vape and, if so, what they have vaped in order to properly diagnose the problem and provide the best treatment. When we have patients experiencing serious pulmonary effects after vaping, we work closely with the Regional Center for Poison Control and Prevention and the Department of Public Health. Toxicology and public health expertise is critical to educate us on the toxicity of certain substances so we can respond in the most effective way and better understand the causes of pulmonary injury in the long term.
3. It’s crucial to follow vaping trends and terminology to respond to the current situation.
In order to understand what our youths are using, it is important to use the current terminology to ask questions about vaping practices. If we do not ask the questions in a manner that captures current trends, then an adolescent may not report what is going on. Understanding youth perceptions is also key to education and prevention. There is so much information and misinformation/inaccurate claims on social media platforms. In addition, the vaping industry has the resources to directly influence our youth through unregulated campaigns.
Our trainees are very adept at figuring out the latest trends among youth and the social media influences surrounding vaping, which helps us to better ask about these issues using the terminology that will get us the information needed and more effectively share the dangers of vaping in a way that will resonate with our young population. One of our fellows developed a vaping use survey of youth that we hope will help us to understand and track local practices more closely.
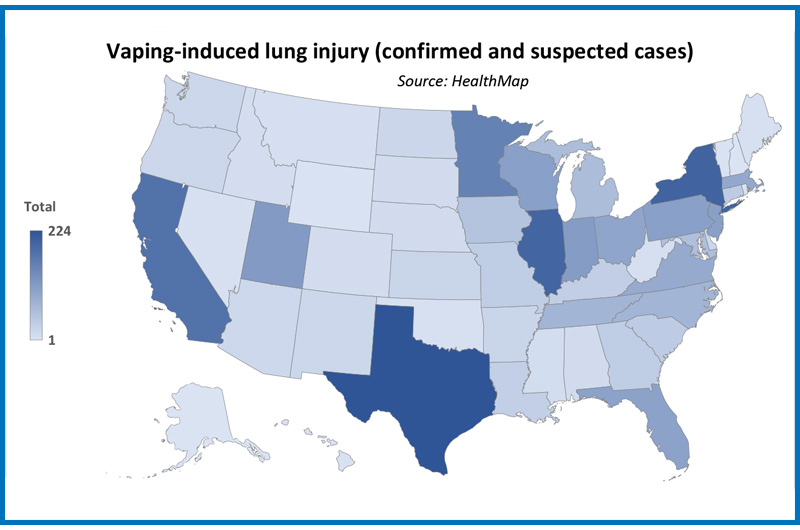
as of Dec. 12, 2019.
( HealthMap: Yulin Hswen and John S. Brownstein, Boston Children’s Hospital, Harvard Medical School)
Researchers at Boston Children’s are also collecting data using HealthMap digital disease surveillance platform to gain a better understanding of the epidemic.
4. Educating others can be an important strategy to ultimately prevent vaping.
We have been proactive in educating health care professionals, parents, educators, and students about the dangers of vaping. This includes publishing articles on vaping in medical journals and sharing our expertise through presentations at schools, hospitals, and professional organizations in the hopes of raising awareness about the broad impact vaping has on teens, including not only the health effects but also the psychological and social impacts. Our goal is to discourage more youth from vaping.
5. Pulmonary specialists can play a powerful role in advocating for better policies to protect our youth from vaping-related illnesses.
Clinicians and specialists all over the country need to be strong advocates for tougher e-cigarette policies in their states. For instance, our experts at Boston Children’s helped to advise Massachusetts Governor Charlie Baker, the Department of Public Health, and the Massachusetts Health Council about the dangers of vaping, and were instrumental in Massachusetts becoming the first state to impose a temporary ban on the sale of all e-cigarettes and vape products. Ultimately, Massachusetts passed a comprehensive law (effective in June 2020) prohibiting the sale of all flavored tobacco products, including menthol cigarettes and vape products.
To get involved in existing efforts in your region, look to organizations like the American Academy of Pediatrics and American Thoracic Society.
Learn more
If you are a clinician and want to refer a patient: call our page operator at 617-355-6369 and page 8273 (VAPE). You can also send a note to vaping@childrens.harvard.edu for non-urgent questions.
If you are a patient or parent with concerns about pulmonary issues associated with vaping, please discuss referral to our program with your primary care provider.
Contact our Division of Pulmonary Medicine.
Related Posts :
-

Ductus arteriosus stenting could help severely ill infants with pulmonary arterial hypertension
Treatment for infants who have severe pulmonary arterial hypertension (PAH) is sometimes limited. Because they haven’t physically ...
-

New hospital discharge practices could improve health of infants with bronchopulmonary dysplasia
The chronic lung disease bronchopulmonary dysplasia (BPD) affects a significant number of infants who were born early and ...
-

Five ways to help manage your child’s asthma this school year
While fall is a time of considerable change for children — a new school year with new challenges — it can also ...
-

Finding a way to help newborns who can’t immediately have heart treatment
Newborns with complex congenital heart defects (CHD) and pulmonary overcirculation often need treatment as soon as possible. Unfortunately, ...